This site is intended only for the use of UK Healthcare Professionals
Enteral Nutrition
Article
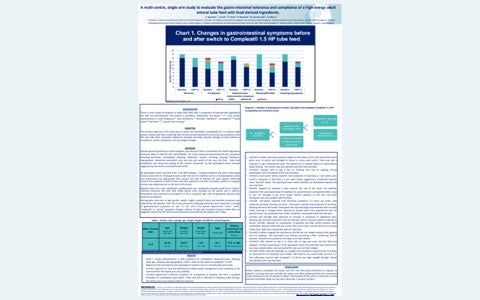
A multi-centre, single arm study to evaluate the gastro-intestinal tolerance and compliance of a high energy adult enteral tube feed with food derived ingredients.
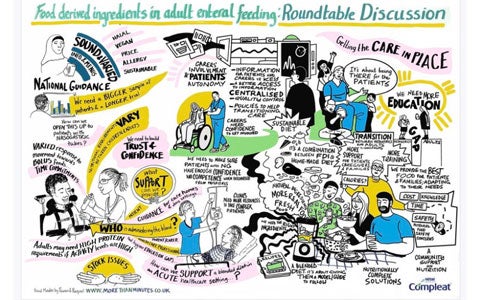
New Directions in Home Enteral Feeding: Are food-derived ingredients changing the landscape? Expert dietitians share their views in a recorded roundtable discussion.
The webinar was live in February 2024. The speakers discussed the Real-World Evidence for children with neuro-disabilities who have low energy expenditure coupled with feed intolerances may benefit from a low-energy hydrolysed enteral formula to minimise the risk of excessive weight gain, further compromising mobility and obesogenic complications.
The prevalence of children with complex neuro-disability has increased due to advances in the medical management of preterm infants and improved care for children with severe neurological impairment . Neuro-disability covers a wide range of clinical conditions, including acquired brain injury, epilepsy and learning disability. Neuro-disabilities present a significant disease burden for the child and family, with the focus for families to promote the best possible participation in life for all affected. Children with neuro-disabilities can be significantly disadvantaged in their ability to nourish themselves due to poor hand to mouth motor coordination, along with disordered swallowing, resulting in aspiration of food in the lungs. The length of feeding time may be considerably increased and instead of mealtimes being an enjoyable experience, they are distressing for both child and carer. These impairments in feeding eventually lead to undernutrition and invariably children require a feeding tube to ensure nutritional requirements are met. Although tube feeding improves overall nutritional status, it has also been associated with an excess deposition of body fat compared with typically developing children. Children with neuro-disability are at risk of becoming overweight because of their low activity and psychosocial constraints. Additionally, children with a neuro-disability tend to grow slowly for non-nutritional reasons and have altered body composition due to underdeveloped skeletal muscle. Children are more likely to be overweight and tend to have low lean muscle mass - therefore a low BMI in this group does not necessarily imply low fat stores. Efforts are needed to protect severely disabled children from overfeeding and to help families of children with neuro-disabilities to manage their child’s weight. Children with neuro-disabilities who are fed to 80% of their estimated average energy requirements have reported a positive energy balance resulting in high body fat mass. Of note, any attempt to dilute the existing proprietary feeds to reduce the calorie intake to a level commensurate with the energy expenditure of a child with a disability is likely to have an adverse impact on micronutrient and protein intake. The clinical nutrition industry has responded to this need and developed commercially available enteral formulas that are low in energy but nutritionally adequate for protein and micronutrients, essential for developing children who are reliant on enteral formula to supply a major proportion of their intake [8]. Additionally, feed tolerance is generally worse in children with neuro-disabilities, associated with comorbidities including epilepsy, posture and tone disorders, and medications used for the treatment of these conditions can further exacerbate gastrointestinal function. Common feed related symptoms associated with neuro-disabilities include vomiting, retching, pain associated with feeding - feedinduced dystonia, constipation, and gastrointestinal dysmotility. The aim of this national multicentre retrospective study was to monitor the effectiveness of a low energy hydrolysed enteral formula on weight management, feed tolerance and health economics in children with a neuro-disability.
A hub of tube feeding support and guidance for parents & carers of tube fed children. Talking Tube Feeding features informative articles written by healthcare professionals, inspiring stories shared by tube feeding families, and even blended diet recipes created by a dietitian. Share with your families today! All Talking Tube Feeding articles and videos have been created in partnership with healthcare professionals and tube feeding families, aiming to offer credible tube feeding information. Visit Now Highlights include Andie & Ava's Story - 3 part video series 10+ Blended Diet recipes written by a paediatric dietitian Tube feeding glossary & equipment guide Transitioning to adult care Share with your patients' families today! www.talkingtubefeeding.com Contribute to Talking Tube Feeding We’re always looking for healthcare professionals to contribute their expertise to the Talking Tube Feeding website. So, if you have an interesting topic suggestion, get in touch at: talkingtubefeeding@uk.nestle.com Connecting with Families If you think your families would like to share their tube feeding experiences on Talking Tube Feeding, please contact us on: talkingtubefeeding@uk.nestle.com. We can work flexibly with families, whether they want to contribute quotes/recommendations or a full diary-style feature. To order Talking Tube Feeding pens and leaflets for your families, please contact your Nestlé Health Science representative.
Dr Graeme O’Connor from Great Ormond Street Hospital, London, UK explores the use of blended tube feeds in detail, covering microbiomes and dysbiosis, tolerance and the role of short chain fatty acids, while sharing his own clinical experience of using feeds containing food-derived ingredients.
Published in HSOA Journal of Neonatology and Clinical PediatricsThis case study series provides an overview of four children aged between twenty-six months to ten years. The children have a range of conditions including learning and physical disabilities, digestive tract abnormalities and genetic conditions such as DiGeorge’s syndrome. Reflux, constipation and vomiting were among the symptoms of feed intolerance reported. Significant improvements in these symptoms were reported following a change to Compleat Paediatric®; a 1.2 kcal/ ml formula with 14% food derived ingredients (Nestlé Health Science), which resulted in improved quality of life for children and their families. Compleat Paediatric® could be considered as a sole source of nutrition or in conjunction with BD when children are not tolerating a standard commercial formula.Case studies provided by;Aneeqa Siddiqui, Paediatric Dietitian, Birmingham Women’s and Children’s NHS FoundationTrust, Birmingham, UKVictoria Steele, Senior Specialist Dietitian, Friarage Hospital, Northallerton, UKMarti van der Linde, Community Paediatric Dietitian, Worcestershire North, Nutrition and Dietetic teamOrder Samples
Watch our webinars here: Emerging Trends in Blended Diets 1 Year on – Evidence & Clinical Practice The third webinar in the series has four experienced clinicians talk about their experiences of transitioning paediatric patients to a blended diet, as well as, a tube feeding formula with food-derived ingredients. Our speakers dive into the anatomy of why providing a blended diet may be better tolerated than a standard tube feed, as well as the process and multi-disciplinary team approach in creating and implementing a blended diet policy. Followed by an engaging Q&A with the audience. Speakers; Kate Samela, Dr Mohamed Mutalib, Marie Watson and Naheeda Habib A Practical Implementation of Blended Diets for Healthcare Professionals The second webinar in the series, focuses specifically on the practical challenges that Healthcare Professionals face in supporting parents, carers and families through their journey in using blended diets as a source of nutrition for their child. Our speakers discuss feeding tubes, risk assessments and how they have successfully introduced blended diets to their patients. Speakers; Dr Su Bunn, Denise Kennedy, Vicki Steele and Clare Armstrong The Emerging Trend of Blended Diets; Sharing Best Practice Amongst Healthcare Professionals Our first webinar dives into the emerging trend of blended diets for enteral feeding. Our speakers discuss how blended diets may change the way we think about tube feeding and compare with the USA, who are leading the way when it comes to blended diets and food-based formulas. We hear about the positive move made by the British Dietetic Association in their updated guidance on blended diets and hear about the growing evidence for a newly available prescribed feed that contains food-derived ingredients. Speakers; Gerard Minor, Dr Clare Thornton-Wood, Jayne Lewis
Recently, as reported by dietetic departments in the United Kingdom, we have seen an increase in Homemade Blended Diets (HBD) being given to children requiring tube feeding. HBD practice may increase the risk of tube occlusion and nutritional inadequacies. In 2015 the British Dietetic Association (BDA) developed their first ‘Practice toolkit liquidised food via gastrostomy tube’, whic...
This checklist can be used when transitioning a child onto a blended diet, using Compleat® paediatric as a base in recipes. Use this resource as a blended diet risk assessment and agreement between parents/carers and dietitian.
Critical illness is often associated with catabolism. Consequently, providing nutritional support to those who cannot eat is essential to prevent malnutrition in the critical care setting.1 When considering nutrition support in the critical care unit (ICU), certain comorbidities should be taken into careful consideration when formulating an enteral feeding plan. For exa...
Many patients requiring long term enteral nutrition have neurological disorders, such as motor neurone disease (MND) or Huntington’s disease (HD). In our experience, a proportion of these individuals may struggle to tolerate enteral feeding despite optimising medical management and excluding obvious gastrointestinal pathology. In MND, prolonged reduced mobility, weaknes...
This case study discusses the nutritional management of a severely undernourished patient with head and neck cancer. The patient experienced diarrhoea and significant weight loss, despite the use of various enteral formulas and delivery methods (continuous and bolus feeding). Thereafter a combination of products within the Peptamen® range were trialled. A marked reduction i...
Major trauma refers to significant or multiple injuries that could result in death or severe disability, sustained from a traumatic insult such as a road traffic collision, fall, sporting accident, or physical assault. It is the leading cause of death and major disability in people aged under 45 years in the UK.1 Critically injured patients are often managed on ...
GEORGE IS A 63 YEAR OLD MARRIED MAN WHO WAS DIAGNOSED WITH MALIGNANT NEOPLASM OF THE OESOPHAGUS IN SEPTEMBER 2011. A two stage oesophago-gastrectomy was performed in February 2012 with a jejunal tube inserted for feeding. The patient reported that during his hospital stay he was given a polymeric feed via the jejunostomy. He suffered with severe diarrhoea for the length of his hospital stay. He was discharged home in April 2012, taking small meals and snacks without enteral nutrition. Over a 6 mo...
Introduction/overview Chronic pancreatitis is a progressive and irreversible inflammatory disease of the pancreas. This results in exocrine and endocrine dysfunction which in time leads to maldigestion and malabsorption reducing the body’s ability to utilise essential macro and micronutrients. Consequently protein energy malnutrition is common. Research indicates that in more than 80...
This case study discusses the nutritional management of a critically ill patient with a traumatic brain injury (TBI). Due to poor tolerance of gastric feeding, his nutritional requirements could not be met using a polymeric formula. His feed was changed to Peptamen® HN (a 100% whey peptide feed) and enteral absorption improved, allowing his full nutritional requirements to b...
Human immunodeficiency virus (HIV) is a virus that attacks the immune system specifically targeting CD4 cells, white blood cells which play a major role in protecting against infection. As the virus progresses and the CD4 count decreases there is an increased risk of certain infections referred to as ‘opportunistic infections’ (OIs). The gastrointestinal (GI) tr...
"ENTERAL TUBE FORMULA: A MULTICENTRE TRIAL IN THE UNITED KINGDOM The prevalence of Cerebral Palsy (CP) children who require a low-calorie feed is between 8-15%. ESPGHAN working group recommend using a low-fat, low-calorie, high fibre, micronutrient replete formula for immobile Neurological Impaired children. Children aged 1-11 years with neurological issues were recruited from UK National Health Service (NHS). Participants were given the new low-c..."
Kathyrn Simpson, Paediatric Dietitian, worked with 8 of her families for the acceptability and tolerance study for Peptamen Junior 1.5. Hear about Kathryn’s experience of being involved in the trial and in particular, learn about two children who took part. Case study 1 focuses on a 6 year old girl with complex TOF and OA. Case study 2 is an 8 year old girl with Cockayne Syndrome.
This webinar had the focus on the use of fibre supplements' in the nutritional management of patients with acute illness. The speaker, Nirouz Zarroug, discussed the impact of clinical decisions related to patient care.
Published in HSOA Journal of Neonatology and Clinical PediatricsThis case study series provides an overview of four children aged between twenty-six months to ten years. The children have a range of conditions including learning and physical disabilities, digestive tract abnormalities and genetic conditions such as DiGeorge’s syndrome. Reflux, constipation and vomiting were among the symptoms of feed intolerance reported. Significant improvements in these symptoms were reported following a change to Compleat Paediatric®; a 1.2 kcal/ ml formula with 14% food derived ingredients (Nestlé Health Science), which resulted in improved quality of life for children and their families. Compleat Paediatric® could be considered as a sole source of nutrition or in conjunction with BD when children are not tolerating a standard commercial formula.Case studies provided by;Aneeqa Siddiqui, Paediatric Dietitian, Birmingham Women’s and Children’s NHS FoundationTrust, Birmingham, UKVictoria Steele, Senior Specialist Dietitian, Friarage Hospital, Northallerton, UKMarti van der Linde, Community Paediatric Dietitian, Worcestershire North, Nutrition and Dietetic teamOrder Samples
Recently, as reported by dietetic departments in the United Kingdom, we have seen an increase in Homemade Blended Diets (HBD) being given to children requiring tube feeding. HBD practice may increase the risk of tube occlusion and nutritional inadequacies. In 2015 the British Dietetic Association (BDA) developed their first ‘Practice toolkit liquidised food via gastrostomy tube’, whic...
New Directions in Home Enteral Feeding: Are food-derived ingredients changing the landscape? Expert dietitians share their views in a recorded roundtable discussion. Join us as we watch back Episode 1, the first instalment in a 3-part series of short lunchtime webinars where home enteral feeding dietitians discuss their current practice and challenges as well as the clinical evidence for food derived ingredients in enteral nutrition formulas and where they see their use changing dietetic practice and expanding options for patients. You can watch episode 2 here. And episode 3 here. Chairperson: Stephanie Wakefield, Specialist Upper GI Dietitian and Lecturer in Human Nutrition & Dietetics, Newcastle Upon Tyne Hospitals, Newcastle University Speakers: Adrian Gilson, Band 7 Community Nutrition Support Dietitian Jamie Leung, Lewisham Healthcare NHS Trust, Department of Paediatrics Karen Voas-Wootton, Glan Clwyd Hospital, Adult Team Lead Kirsty Capper, Chester Adult Community, Adult Team Lead Hannah Meanwell, Nottingham Hospital, Adult HEF Dietitian
New Directions in Home Enteral Feeding: Are food-derived ingredients changing the landscape? Expert dietitians share their views in a recorded roundtable discussion. Join us as we watch back Episode 2, the second instalment in a 3-part series of short lunchtime webinars where home enteral feeding dietitians discuss their current practice and challenges as well as the clinical evidence for food derived ingredients in enteral nutrition formulas and where they see their use changing dietetic practice and expanding options for patients. You can watch episode 1 here. And episode 3 here. Chairperson: Stephanie Wakefield, Specialist Upper GI Dietitian and Lecturer in Human Nutrition & Dietetics, Newcastle Upon Tyne Hospitals, Newcastle University Speakers: Adrian Gilson, Band 7 Community Nutrition Support Dietitian Jamie Leung, Lewisham Healthcare NHS Trust, Department of Paediatrics Karen Voas-Wootton, Glan Clwyd Hospital, Adult Team Lead Kirsty Capper, Chester Adult Community, Adult Team Lead Hannah Meanwell, Nottingham Hospital, Adult HEF Dietitian
New Directions in Home Enteral Feeding: Are food-derived ingredients changing the landscape? Expert dietitians share their views in a recorded roundtable discussion. Join us as we watch back Episode 3, the third and final instalment in a 3-part series of short lunchtime webinars where home enteral feeding dietitians discuss their current practice and challenges as well as the clinical evidence for food derived ingredients in enteral nutrition formulas and where they see their use changing dietetic practice and expanding options for patients. You can watch episode 1 here. And episode 2 here. Chairperson: Stephanie Wakefield, Specialist Upper GI Dietitian and Lecturer in Human Nutrition & Dietetics, Newcastle Upon Tyne Hospitals, Newcastle University Speakers: Adrian Gilson, Band 7 Community Nutrition Support Dietitian Jamie Leung, Lewisham Healthcare NHS Trust, Department of Paediatrics Karen Voas-Wootton, Glan Clwyd Hospital, Adult Team Lead Kirsty Capper, Chester Adult Community, Adult Team Lead Hannah Meanwell, Nottingham Hospital, Adult HEF Dietitian
Watch our panel discussion hosted by four experienced dietitians, who together explore how best to manage energy requirements amongst children with a variety of conditions, answering questions sent in by other healthcare professionals.
Learn more about MCTs and their role in reducing fat malabsorption
Learn about how to support patients through the home-made blended diet journey alongside a tube feed with food-derived ingredients and new data in adults using food-derived ingredients. To know and download the poster please follow this link Study to evaluate the gastrointestinal tolerance | N+ Hub. for more information on the product Compleat® 1.5 HP for professionals | Nestlé Health Science.
Join the Expert Speaker who will discuss different approaches to Nutrition Management. The speakers will be discussing the impact of clinical decisions related to the nutritional care of patients, in terms of improving outcomes.
GEORGE IS A 63 YEAR OLD MARRIED MAN WHO WAS DIAGNOSED WITH MALIGNANT NEOPLASM OF THE OESOPHAGUS IN SEPTEMBER 2011. A two stage oesophago-gastrectomy was performed in February 2012 with a jejunal tube inserted for feeding. The patient reported that during his hospital stay he was given a polymeric feed via the jejunostomy. He suffered with severe diarrhoea for the length of his hospital stay. He was discharged home in April 2012, taking small meals and snacks without enteral nutrition. Over a 6 mo...