Synopsis:
This case study discusses the nutritional management of a severely undernourished patient with head and neck cancer. The patient experienced diarrhoea and significant weight loss, despite the use of various enteral formulas and delivery methods (continuous and bolus feeding). Thereafter a combination of products within the Peptamen® range were trialled. A marked reduction in diarrhoea was noted, which improved his quality of life and nutritional status. His BMI also increased from 16.9kg/m2 to 20.5kg/m2.
Introduction
Head and Neck Cancers are the fifth most common cancers diagnosed in Scotland1 and it has been identified that early nutritional intervention and support for head and neck cancer patients can impact on their treatment outcome and quality of life.2,3 Patients who are discharged home on tube feeding in Lothian are supported by the Community Enteral Nutrition Team (CENT), who aim to tailor feeding regimens to suit the patient’s needs and ensure their feed is tolerated at all times.
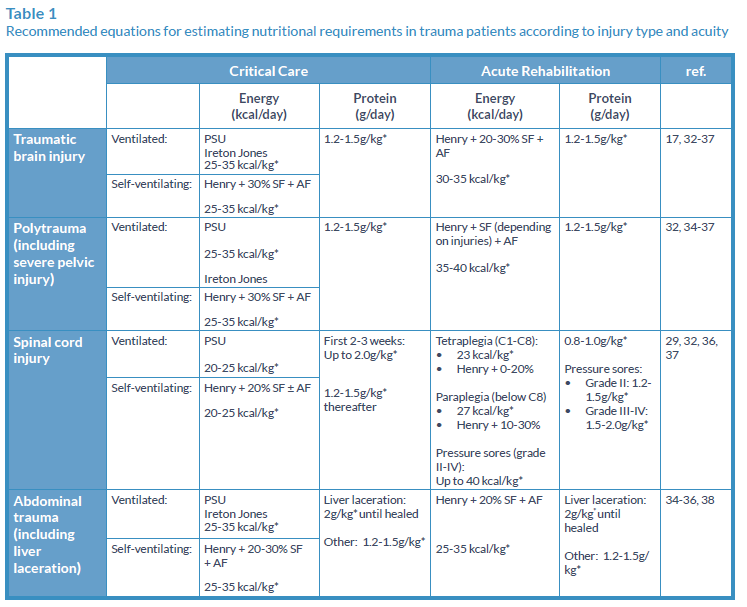
Table 1
Nutritional History
The CENT team received a referral for Mr X following his discharge from hospital. He had lost approximately 10% of his body weight in 4 months, which is clinically significant,4 due to difficulties swallowing prior to diagnosis.
Mr X was due to commence medical treatment for his tongue cancer, and because of the extensive surgery he was to receive (bilateral neck dissection, subtotal glossectomy and reconstruction) it was identified that this would affect his swallow and therefore he required enteral feeding, as recommended by NICE (2006).5
A percutaneous endoscopic gastrostomy (PEG) was therefore inserted during his hospital admission for enteral feeding, however he had experienced loose stools (Bristol Type 6/7) when receiving various feeds. This was reportedly happening immediately after he received the pump or bolus feeds which was causing a great deal of distress to Mr X.
Prior to discharge Mr X had trialled numerous different enteral feeds with poor results and was commence on a bolus regimen of Fortisip® Compact which seemed to on a bolus regimen of Fortisip® Compact which seemed to work better than the pump feeding (see Table 2 below for details of enteral feeds trialled in hospital).
Table 2

Initial Nutritional Assessment
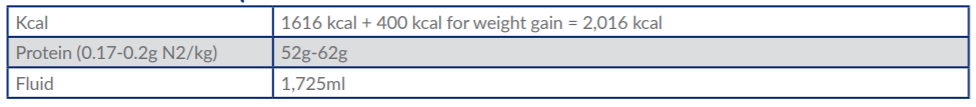
Based on his weight taken on his initial visit (49.3kg), requirements were calculated using Henry (2005) equations as shown below.6
Table 3: Nutritional Requirements
Nutritional Goals and Recommendations
Due to the numerous side effects which can be caused by chemotherapy and radiotherapy, it is important that nutritional intervention is commenced early in the patient’s management, as found by Paccagnella et al (2010).7 Mr X has remained nil by mouth (NBM) due to an unsafe swallow caused by his diagnosis and cancer treatment, therefore he solely relies on his PEG for nutrition, fluids and medications. Therefore, our aim for Mr X was to improve his nutritional status through his PEG, which was inserted during surgery.
Initial Home Visit
At his initial home visit we recommended slowly increasing the Fortisip® Compact boluses, as Mr X seemed to be improving and his wife reported his loose stools were also gradually improving. However, two days later I was notified that the issues with loose stools had returned, therefore we agreed to trial Peptamen® Vanilla bottles 200ml boluses four times daily (providing 800 kcal and 32g protein). Mr X wasn’t keen to be attached to a feeding pump, therefore at that point pump feeding wasn’t an option.
Dietetic Review
1000ml Peptamen® @ 75-125ml/hr overnight (rate to slowly increase over several days) plus 2–3 Peptamen® Vanilla bottles (200ml) bolus feeds daily) (Provides:1,400 -1600 kcal and 56-64g protein)
1000ml Peptamen® HN @ 125ml/hr overnight, plus 3 x 200ml boluses of Peptamen® vanilla bottles daily (Provides: 1,930 kcal and 90g protein)
- Four days after trialling Peptamen®, Mr X’s bowel function had improved significantly, and his loose stools had reduced to twice per day. It was therefore suggested he increased his Peptamen® boluses to 200ml five times daily, providing 1,000 kcal and 40g protein.
- Four days later, Mr X’s stools were becoming more formed, and bowel movements had reduced to once daily. He was keen to try a combination of pump feeding and bolusing. Replicating a meal pattern during the day using the boluses of Peptamen® allowed Mr X to remain a part of his family during meal times which also helped to improve his mood. Therefore the following regimen was prescribed.
- A week later, Mr X’s bowels were only moving every two days, with no further episodes of diarrhoea. In order to increase the calorie and protein provision of his feed without increasing the volume, the feed was changed to:
Rationale for Changing to Peptamen®
Peptamen® was used with Mr X as he had tried numerous different feeds whilst in hospital and showed poor tolerance to both standard and malabsorption specific feeds on our contract. The patient unfortunately refused fibre containing feeds therefore this was not trialled. Peptamen® is a 100% whey peptide feed, and has been found to be tolerated well in those with poor absorption.8,9 As Mr X was experiencing impaired GI function (as evidenced by his loose stools and weight loss) I used my clinical judgement to trial this feed and assessed his tolerance closely. Our team has had numerous successes using Peptamen®, therefore this was a good alternative to trial and Mr X showed clear improvements in his symptoms within four days of trialling Peptamen®.
Discussion: Why did the other products fail to improve symptoms?
The other products may have failed with this particular gentleman due to his impaired GI function, which could have been caused following the extensive surgery he had received, and also the previous chemotherapy and radiotherapy he had received for lung cancer in the past. Fortisip® Compact also has a much higher osmolarity compared to the Peptamen® range of products, which may have affected tolerance. Due to Mr X’s impaired GI function, these types of feed may not have been tolerated well in the small bowel, and may have exacerbated the diarrhoea whenever a feed was trialled. Peptamen®, as a 100% whey peptide feed, may have improved his feeding tolerance due to the hydrolysed proteins and high MCT content.
Conclusion
Following numerous different options of feeding products, Peptamen® has not only improved Mr X’s nutritional status, but has also improved his quality of life. He no longer has to worry about his uncontrolled bowels, and is able to get to work, go on holidays and relax at home. Mr X will require long-term tube feedingas his sole source of nutrition, therefore it is critical that the feed suits his needs. Using the combination of Peptamen®, Peptamen® HN and Peptamen® bottles, we have been able to tailor a regimen which suits him, is well tolerated, and provides him with the required nutrients. By combining the products in the Peptamen® range, it was easier to provide Mr X with his nutritional requirements, without having to provide an excessive amount of feed, which is also more practical for those patients on long-term enteral feeding.
References
- H1. ISD 2015. Cancer in Scotland [online]. [viewed 1 March 2016]. Available from: http://www.isdscotland.org/Health-Topics/Cancer/ Publications/2015-04-28/Cancer_in_Scotland_summary_m.pdf.
- ISENRING, EA., CAPRA, S & BAUER, JD. 2004. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. British Journal of Cancer. [online]. June, Vol 91, pp447-452. [Viewed 15 March 2016]. Available from: http://www.ncbi.nlm.nih. gov/pmc/articles/PMC2409852/pdf/91-6601962a.pdf.
- SIGN 2006. Diagnosis and management of head and neck cancer: A national clinical guideline. [online]. Edinburgh: SIGN. PP. 1-35. [viewed 4 March 2016]. Available from: http://www.sign.ac.uk/pdf/sign90.pdf.
- ELIA, M. 2003. The MUST report, nutritional screening of adults: A multidisciplinary responsibility. Development and use of MUST for adults. BAPEN.
- NICE. 2006. Nutrition support for adults: Oral nutrition support, enteral tube feeding and parenteral nutrition http://www.nice.org.uk/guidance/cg32/ chapter/1-Guidance#enteral-tube-feeding-in-hospitaland-the-community.
- HENRY, CJK. 2005. Basal metabolic rate studies in humans: Measurement and development of new equations. Public Health Nutrition. Vol 8, No 7a, pp. 1133-1152
- PACCAGNELLA ET AL, C. 2010. Early nutritional intervention improves treatment tolerance and outcomes in head and neck cancer patients undergoing concurrent chemoradiotherapy. Support Care Cancer. [online]. July, Vol 18, Issue 7, pp.837-845. [Viewed 15 March 2016]. Available from: http://rd.springer.com/journal/520/18/7/page/1.
- SALOMON SB, JUNG J, VOSS T, SUGUITAN A, ROWE WB, MADSEN DC. An elemental diet containing mediumchain triglycerides and enzymatically hydrolyzed protein can improve gastrointestinal tolerance in people infected with HIV (1998); 98(4):460-2.
- DYLEWSKI ML, PRELACK K, SHERIDAN R (2006). Whey-based formulas improve tube feeding tolerance in pediatric burn patients. Poster 72. A.S.P.E.N Clinical Nutrition Week.
This case study discusses the nutritional management of a severely undernourished patient with head and neck cancer. The patient experienced diarrhoea and significant weight loss, despite the use of various enteral formulas and delivery methods (continuous and bolus feeding). Thereafter a combination of products within the Peptamen® range were trialled. A marked reduction i...