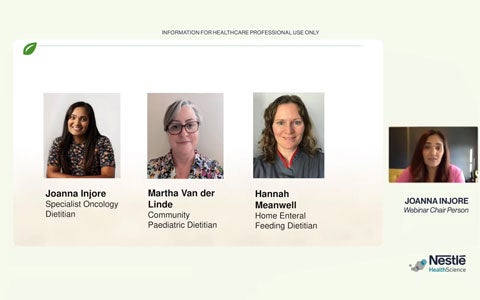
The webinar was live in February 2024. The speakers discussed the Real-World Evidence for children with neuro-disabilities who have low energy expenditure coupled with feed intolerances may benefit from a low-energy hydrolysed enteral formula to minimise the risk of excessive weight gain, further compromising mobility and obesogenic complications.
You can watch the first session “Gastrointestinal implications of neurological impairment” with Rita Shergill-Bonner, RD, Lead Gastroenterology Paediatric Dietitian at Evelina London Children’s Hospital via this link.
You can watch the second session “Impact of a partially hydrolysed low energy enteral formula in children with a neurological impairment gastrointestinal.” with Dr Graeme O’Connor Ph.D. RD MBDA, Research lead for Dietetics at Great Ormond Street Hospital via this link.
You can watch the Q&A session with Rita Shergill-Bonner & Dr Graeme O’Connor, via this link.
To read and download the publication discussed in the session, please click on this link.
To know more on Peptamen Junior 0.6 , please visit his link.
The prevalence of children with complex neuro-disability has increased due to advances in the medical management of preterm infants and improved care for children with severe neurological impairment [1]. Neuro-disability covers a wide range of clinical conditions, including acquired brain injury, epilepsy and learning disability. Neuro-disabilities present a significant disease burden for the child and family, with the focus for families to promote the best possible participation in life for all affected [2].
Children with neuro-disabilities can be significantly disadvantaged in their ability to nourish themselves due to poor hand to mouth motor coordination, along with disordered swallowing, resulting in aspiration of food in the lungs. The length of feeding time may be considerably increased and instead of mealtimes being an enjoyable experience, they are distressing for both child and carer. These impairments in feeding eventually lead to undernutrition and invariably children require a feeding tube to ensure nutritional requirements are met [3].
Although tube feeding improves overall nutritional status, it has also been associated with an excess deposition of body fat compared with typically developing children. Children with neuro-disability are at risk of becoming overweight because of their low activity and psychosocial constraints [4]. Additionally, children with a neuro-disability tend to grow slowly for non-nutritional reasons and have altered body composition due to underdeveloped skeletal muscle. Children are more likely to be overweight and tend to have low lean muscle mass - therefore a low BMI in this group does not necessarily imply low fat stores [5]. Efforts are needed to protect severely disabled children from overfeeding and to help families of children with neuro-disabilities to manage their child’s weight [6].
Bibliography
- Stoll BJ. “Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network”. Pediatrics (2010): 126.
- National Guideline A. “National Institute for Health and Care Excellence: Guidelines”. Cerebral palsy in under 25s: assessment and management. London: National Institute for Health and Care Excellence (NICE) Copyright National Institute for Health and Care Excellence (2017).
- Strand KM., et al. “Growth during infancy and early childhood in children with cerebral palsy: a population-based study”. Developmental Medicine and Child Neurology 58.9 (2016): 924-930.
- Neter JE., et al. “The prevalence of overweight and obesity and its determinants in children with and without disabilities”. The Journal of Pediatrics 158.5 (2011): 735-739.
- Pascoe J., et al. “Body mass index in ambulatory children with cerebral palsy: A cohort study”. Journal of Paediatrics and Child Health 52.4 (2016): 417-421.
- Lip SZL., et al. “Prevalence of under and overweight in children with neurodisability, using body composition measures”. European Journal of Clinical Nutrition 72.10 (2018): 1451-1454.
The webinar was live in February 2024. The speakers discussed the Real-World Evidence for children with neuro-disabilities who have low energy expenditure coupled with feed intolerances may benefit from a low-energy hydrolysed enteral formula to minimise the risk of excessive weight gain, further compromising mobility and obesogenic complications.