L. Rofes*, V. Arreola†, R. Mukherjee‡, J. Swanson§ & P. Clave*,†
*Centro de Investigacion Biomedica en Red de enfermedades hepaticas y digestivas (CIBERehd), Instituto de Salud Carlos III, Barcelona, Spain.
†Unitat de Proves Funcionals Digestives, Department de Cirurgia, Hospital de Mataro, Universitat Autonoma de Barcelona, Mataro, Spain.
‡Nestle Research Center, Nestec Ltd, Lausanne, Switzerland.
§Nestle R&D Center, Nestec Ltd, Minneapolis, MN, USA.
Correspondence to:
Dr P. Clave, Department of Surgery, Hospital de Mataro, Universitat
Autonoma de Barcelona, Carretera de Cirera s/n 08304, Mataro, Spain. E-mail: pere.clave@ciberehd.org
Publication data Submitted 4 February 2014 First decision 17 February 2014 Resubmitted 19 February 2014 Accepted 19 February 2014 EV Pub Online 13 March 2014
This article was accepted for publication after full peer-review
SUMMARY
Background
Increasing bolus viscosity of thin liquids is a basic therapeutic strategy to protect patients with oropharyngeal dysphagia (OD) from aspiration. However, conventional starch thickeners increase postdeglutitive residue.
Aim
To assess the therapeutic effect of a new xanthan gum-based thickener, Resource ThickenUp Clear (Nestle Health Science, Vevey, Switzerland) on patients with oropharyngeal dysphagia.
Methods
We studied the effect of Resource ThickenUp Clear using a clinical method and videofluoroscopy on 120 patients with oropharyngeal dysphagia (66 with stroke, 41 older and 13 with neurodegenerative diseases) and 14 healthy volunteers while swallowing thin-liquid, nectar-like and spoon-thick boluses. We assessed the prevalence of signs of impaired safety and efficacy of swallow and the physiology of the swallow response.
Results
Increasing bolus viscosity with Resource ThickenUp Clear: (i) improved safety of swallow demonstrated by a reduction in the prevalence of cough and voice changes in the clinical study and penetrations and aspirations during video fluoroscopy. Prevalence of aspirations was 12.7% with thin liquid, 7.7% with nectar-like (P < 0.01) and 3.4% with spoon-thick (P < 0.01) viscosities. Penetration–Aspiration Scale was reduced from 3.24 0.18 at thin liquid to 2.20 0.18 at nectar-like (P < 0.001) and to 1.53 0.13 at spoon-thick (P < 0.001) viscosities; (ii) did not enhance pharyngeal residue; (iii) nectar-like viscosity did not affect bolus velocity nor timing of swallow response and (iv) spoon-thick viscosity reduced bolus velocity.
Conclusions
Resource ThickenUp Clear improves the safety of swallow without increasing residue providing a viscosity-dependent therapeutic effect for patients with oropharyngeal dysphagia. At nectar viscosity, the effect is due to intrinsic texture properties, spoon-thick viscosity adding changes in swallow physiology. NCT01158313.
INTRODUCTION
Oropharyngeal dysphagia (OD) is a gastrointestinal motility disorder specifically recognised by the World Health Organization in the International Statistical Classification of Diseases and Related Health Problems ICD-9 and ICD-10.1 OD is a highly prevalent clinical condition, present in up to 50% of patients with neurological diseases and in the elderly. Approximately 50–75% of these dysphagic patients present impaired safety of swallow, with bolus penetrations into the laryngeal vestibule and 20–25% tracheobronchial aspirations during swallow response.2 Delayed laryngeal vestibule (LV) closure is the main mechanism impairing airway protection in patients with neurogenic dysphagia and in the elderly and leads to severe respiratory complications.2 In stroke patients, OD triplicates the relative risk of pneumonia, which increases to 11 times if the patient presents aspirations.3 Aspiration pneumonia is associated with a 3-fold increased risk of death compared with stroke patients without pneumonia.4 In the elderly, OD is also an independent risk factor for the development of lower respiratory tract infections and pneumonia.5–7 The development of evidence-based treatments that increase safety of swallow and protect patients from aspirations is necessary to avoid respiratory complications and improve morbidity and mortality rates of the dysphagic population.8
One of the basic compensatory interventions in hospitals and long-term care facilities to increase the safety of swallow and avoid aspirations is to thicken liquids. Viscosity is a rheological property that measures the fluid’s internal resistance to flow and the rate of flow per unit of force applied. We have previously described how thickening liquids with starch-based thickeners reduced LV penetrations and tracheobronchial aspirations9, 10 with the consequent reduction in the incidence of aspiration pneumonia rates.11 It has been proposed that slowing down bolus velocity through the pharynx is the main action mechanism of thickeners to protect against aspirations.12 However, parallel to its therapeutic effect, enhancing bolus viscosity with starch thickeners increases post-deglutitive oropharyngeal residue, especially in patients with deficient bolus propulsion such as elderly patients and patients with neurodegenerative dis-eases.2, 9, 10 This might increase the risk of post-swallow aspirations.13 Another disadvantage of starch-based thickened liquids is that they are, in general, not well accepted by patients.14
A new generation of thickeners based on xanthan gum has recently been developed to improve on the therapeutic performance and sensory attributes of the starched-based thickeners. The xanthan gum-based thickeners retain the clarity of clear liquids, possess amylase resistance to keep bolus viscosity stable during saliva contact, are able to thicken a wide range of liquids at different temperatures and maintain stable viscosity over time.15 However, their clinical therapeutic effect and their mechanisms of action on patients with OD has not been evaluated yet.
The aim of this study was to assess the therapeutic effect of a xanthan gum-based thickener (Resource ThickenUp Clear, RTUC) on the clinical and videofluoroscopic signs of OD and the swallow function of dysphagic patients to provide research-based clinical practice.16
MATERIAL AND METHODS
Study population
One hundred and twenty patients consecutively referred to the Gastrointestinal Physiology Laboratory of the Hospital de Mataro (Spain) for swallowing evaluation, were prospectively included in the study. Inclusion criteria were: age more than 18 years, history of swallowing difficulties associated with ageing and/or neurological diseases. Exclusion criteria were: allergy to any medication, major respiratory diseases, surgery in the 3 months prior to the study, background of alcohol or drug dependence or participation in another clinical trial 4 weeks prior. Healthy volunteers (HV) (N = 14) were recruited to explore the effect of the xanthan thickener on normal swallow physiology. All participants were informed about the study and gave written consent. The study protocol was approved by the Institutional Review Board of the Hospital de Mataro and was conducted according to the principles and rules laid down in the Declaration of Helsinki and its subsequent amendments. Trial registration: NCT01158313. Demographical, clinical and nutritional characteristics of the study population, as well as severity of dysphagia symptoms, were also collected in all participants.
Experimental design
The effect of different levels of viscosity on the clinical signs and symptoms of OD was assessed by a clinical test with high diagnostic accuracy, the Volume-Viscosity Swallow Test (V-VST). The effect on videofluoroscopic signs and the swallow response was assessed by videofluoroscopy (VFS).
Clinical test
The V-VST was performed as described elsewhere.17 Briefly, the patients’ ability to swallow boluses of different volumes (5, 10 and 20 mL) and viscosities (thin liquid, nectar-like, spoon thick) were evaluated in all patients. In addition, to evaluate the minimum amount of thickener needed for each patient, the subgroup of patients that presented impaired safety of swallow at nectar viscosity but safe swallow and residue at spoon-thick viscosity was evaluated with two additional intermediate viscosities: conservative spoon thick and honey, using the algorithm described elsewhere.17
Clinical signs of OD. Signs of impaired efficacy of swallow, such as impaired labial seal, oral residue and piece-meal deglutition (multiple swallows per bolus), symptoms of pharyngeal residue and signs of impaired safety of swallow, such as changes in voice quality (including wet voice), cough and decrease in oxygen saturation ≥3% (measured with a finger pulseoximeter; Nellcor OxiMax, Philips Medical Systems, Eindhoven, Netherlands) were evaluated for each swallow.18
Videofluoroscopy
All patients were imaged for the videofluoroscopic study while seated in a lateral projection which included the oral cavity, pharynx, larynx and cervical oesophagus. Videofluoroscopic recordings were obtained by using a Super XT-20 Toshiba Intensifier (Toshiba Medical Systems Europe, Zoetermeer, The Netherlands) and recorded at 25 frames/s using a Panasonic AG DVX-100B video camera (Matsushita Electric Industrial Co, Osaka, Japan). Digitisation, analysis and measurements of videofluoroscopic images were made using the software Swallowing Observer (Image and Physiology SL, Barcelona, Spain) by an expert clinician not blinded to the viscosity of the bolus. For the videofluoroscopic study, we used the same exploration algorithm as for the V-VST.17
VFS signs. Impairment in the efficacy of swallow was considered when at least one of the following signs was identified during the VFS study: impaired labial seal, the presence/absence of oral residue, pharyngeal residue or piecemeal deglutition and impairment in the safety of swallow was considered when a penetration or an aspiration was detected. The penetrations and aspirations were classified according to the Penetration–Aspiration Scale (PAS).19
Timing of swallow response. Quantitative measurements of the effect of the thickener (Resource ThickenUp Clear; Nestle Health Science, Vevey, Switzerland) on oropharyngeal swallow response were obtained during 5-mL swallows at each viscosity during VFS studies. Timing of opening and closing of glossopalatal junction (GPJ), velopharyngeal junction (VPJ), laryngeal vestibule (LV) and UES were measured, GPJ opening being given the time value 0.
Bolus kinematics. Mean bolus velocity (m/s) acquired by the bolus during the transit between the GPJ and the UES was also calculated.
Bolus rheology
The viscosities used during V-VST and VFS were prepared according to the descriptors of the National Dysphagia Diet Task Force, 1–50 mPa s for thin liquid, 51–350 mPa s for nectar-like, 351–1750 mPa s for honey and conservative spoon thick and >1750 mPa s for spoon-thick viscosity.20 For V-VST studies, thin viscosity was obtained by using mineral water at room temperature, nectar-like viscosity by adding 1.2 g of thickener (Resource ThickenUp Clear, Nestle Health Science) to 100 mL mineral water and spoon-thick viscosity by adding 6 g of thickener to 100 mL mineral water. Honey viscosity was obtained by adding 2.4 g of thickener, and conservative spoon thick by adding 3.6 g, to 100 mL mineral water. Solutions were prepared 5 min before the test. According to the study protocol, the specific levels of viscosity obtained were 21 mPa s for thin liquids, 238 mPa s for nectar and 1840 mPa s for EST.17 For VFS studies, thin viscosity was obtained by mixing 1:1 mineral water and the X-ray contrast Gastrografin (Bayer Hispania SL, Sant Joan Despı, Spain) both at room temperature, nectar viscosity by adding 2.4 g of the thickener to the liquid solution containing the X-Ray contrast and the spoon-thick viscosity by adding 5.4 g of the thickener. Honey viscosity was obtained by adding 3.7 g of thickener to 100 mL of the X-Ray contrast solution and conservative spoon thick by adding 4.4 g. The solutions for VFS studies were prepared 3 h prior the videofluoroscopic examination to obtain equivalent viscosities to those used during the V-VST.15 Boluses of 5, 10 and 20 mL of each viscosity were carefully given to patients with a syringe during both V-VST and VFS studies to ensure accurate measurement of bolus volume.
Product safety
Any adverse events (AEs) occurring during the study and until 1 week after the completion of the study procedures (checked by a telephone call) were documented, assessed for severity and relationship with the study product and classified according to the WHO System Organ Class.
Data analysis and statistical methods
Qualitative parameters were described by relative and absolute frequencies and were compared by the Fisher’s exact test for independent variables or McNemar’s test for paired variables. Quantitative parameters were described by mean SEM and compared by the non-parametric Mann–Whitney U-test or Kruskal–Wallis test for paired variables. Differences between viscosities at each volume were tested using the Cochran’s Q test. If the P value was less than 5% then each viscosity level was tested against the thin-liquid viscosity using McNemar’s test corrected for multiplicity (Bonferroni adjusted). Statistical significance was accepted if P values were <0.05. Statistical analysis was performed using the stats package in R version 2.15 (www.r-project.org).
RESULTS
Study population
The recruitment of participants was carried out between June 2010 and June 2011. Demographical, clinical data and nutritional risk of the study population are described in Table 1. Up to 55% (66) of patients presented OD associated to a previous stroke, 34.2% (41) to ageing and 10.8% (13) to neurodegenerative diseases [mainly Parkin-son’s disease (3) and multiple sclerosis (3)]. Sixty per cent (72) of patients were taking one or more drugs with potential effects on swallow function: 39 were taking anti-depressants; 29, anxiolytics; 17, anti-epileptics; 10, sedatives and five, anti-psychotics.
Effect of RTUC on clinical signs and symptoms of OD
Healthy volunteers. Safety of swallow: Only one healthy volunteer presented a voice change after the deglutition of 20 mL of thin liquid and 20 mL of nectar but not at spoon-thick viscosity. None of the HV presented cough or decreased oxygen saturation at any of the studied viscosities.
Efficacy of swallow: All the HV presented adequate labial seal and were able to swallow all the boluses offered in a single swallow. One healthy volunteer presented oral and pharyngeal residue at spoon-thick viscosity.
Patients. Prevalence of clinical signs of impaired efficacy and safety of swallow in patients with OD at each viscosity series was very high and is depicted in Figure 1.
Table 1
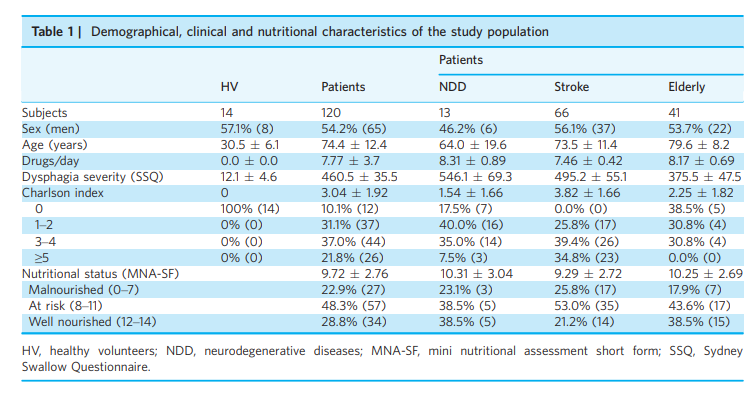
HV, healthy volunteers; NDD, neurodegenerative diseases; MNA-SF, mini nutritional assessment short form; SSQ, Sydney Swallow Questionnaire.
Figure 1
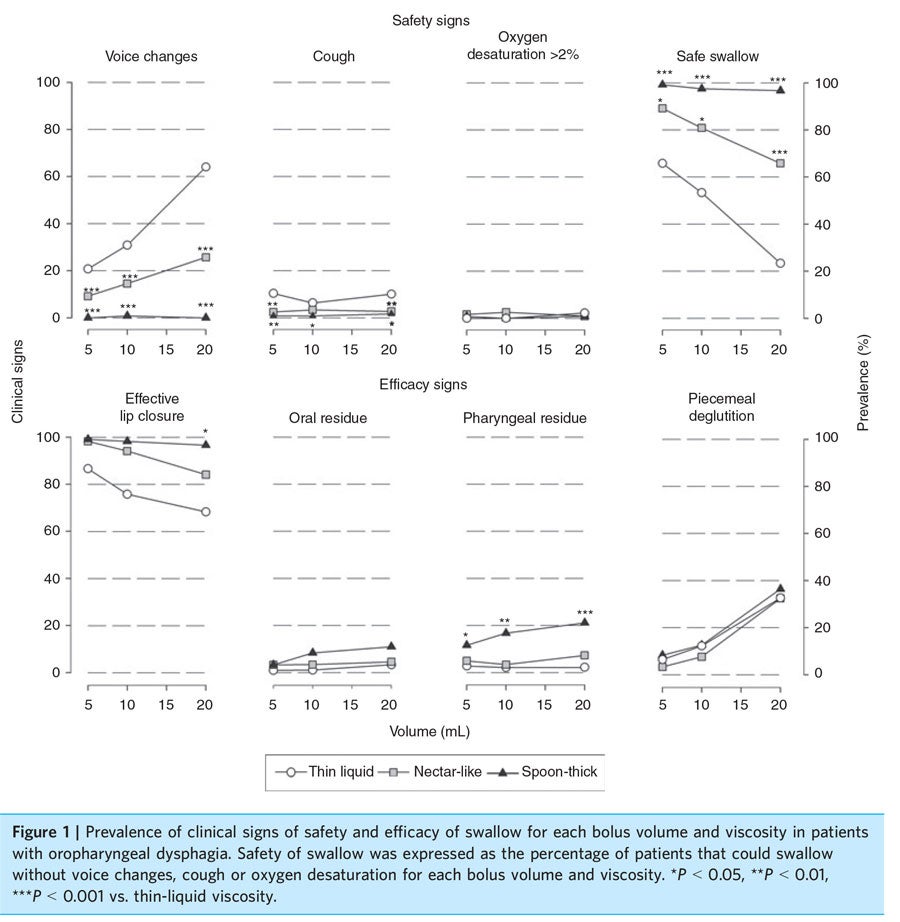
Safety of swallow: Only 20.8% of patients were able to complete the thin-liquid series safely. Up to 60.8% of patients completed the nectar series without presenting any sign of impaired safety of swallow (P < 0.001 vs. thin liquid) and up to 95.8% safely completed the spoon-thick series (P < 0.001 vs. nectar-like).
Efficacy of swallow: Increasing thin-liquid viscosity to spoon thick improved the labial seal efficacy of dysphagic patients (P < 0.05), did not change the prevalence of oral residue or piecemeal deglutition and increased the prevalence of pharyngeal residue symptoms by 18.9% (P < 0.05) (Figure 1).
Intermediate viscosities: Conservative spoon-thick viscosity was administered to 31 patients with impaired safety at nectar and safe swallow but residue at spoon-thick viscosity. Of those, six presented signs of impaired safety and 22 symptoms of pharyngeal residue. Honey viscosity was evaluated in 27 patients; five of them presented signs of impaired safety and 14 reported pharyngeal residue.
Effect of RTUC on videofluoroscopic signs of OD Healthy volunteers. Safety of swallow: Two HV presented nonpathological penetrations into the LV during the deglutition of thin-liquid swallows (score 2 in the PAS) while none of them presented penetrations or aspirations during the deglutition of nectar and spoon-thick viscosities.
Efficacy of swallow: Two of the HV presented mild oral residue at liquid and spoon-thick viscosities and three at nectar-like viscosity. None of them presented pharyngeal residue at any of the viscosities tested.
Patients. Prevalence of videofluoroscopic signs of impaired efficacy and safety of swallow is shown in Figure 2.
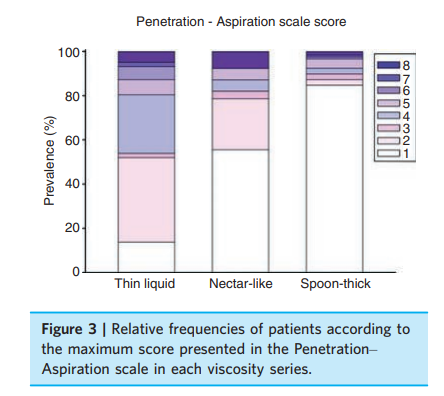
Safety of swallow: Increasing bolus viscosity with the xanthan gum thickener significantly increased the prevalence of patients able to swallow safely from 23.72% at thin-liquid viscosity series to 55.08% at nectar viscosity (P < 0.001) and to 84.74% at spoon-thick viscosity series (P < 0.001). Figure 3 showed distribution of patients according to the maximum score presented in the PAS at each viscosity. It should be noted that prevalence of patients with clinically significant penetrations (scores 3–5) was reduced from 35.3% during thin-liquid series to 13.7% at nectar-like viscosity (P < 0.01) and to 9.3% at spoon-thick (P < 0.01). Prevalence of patients with aspirations (scores 6–8) was reduced from 12.7% during thin-liquid series to 7.7% at nectar (P < 0.01) and to 3.4% at spoon thick (P < 0.01). The mean score of the PAS was reduced from 3.24 0.18 at thin liquid to 2.20 0.18 at nectar (P < 0.001) and to 1.53 0.13 at spoon thick (P < 0.001).
Efficacy of swallow: At thin-liquid viscosity, 12.6% of patients presented significant oral residue and 14.6% presented pharyngeal residue. Increasing bolus viscosity with the xanthan gum thickener did not significantly modify the prevalence of oral, vallecular nor pyriform sinus residue (P > 0.05) (Figure 2).
Intermediate viscosities: Conservative spoon-thick viscosity was tested in 21 patients with impaired safety at nectar and safe swallow with residue at spoon-thick viscosity. Of those, five still presented penetrations; 10, oral residue and 17, pharyngeal residue. Honey viscosity was also evaluated in 21 patients; three of them presented penetrations at the laryngeal vestibule, one presented an aspiration. Oral residue was present in 10 patients and pharyngeal residue in 17.
Effect of RTUC on oropharyngeal physiology
Healthy volunteers. Timing of swallow response: Total duration of swallow (time from GPJ opening to LV opening) of HV during 5-mL thin-liquid swallow was 742.9 29.9 ms. The airway closed at 171.4 12.2 ms and the UES opened at 220.0 16.6 ms. Increasing bolus viscosity to nectar did not significantly affect time to LV closure (174.3 11.6 ms, P > 0.05) and opening (722.9 22.4 ms, P > 0.05) nor UES opening (234.3 8.2 ms, P > 0.05). However, increasing bolus viscosity to spoon thick delayed time to LV closure and UES opening to 230.8 11.2 ms (P = 0.003 vs. thin liquid) and 283.1 11.5 ms (P = 0.003 vs. thin liquid) respectively, but not time to LV opening (P = 0.261 vs. thin liquid).
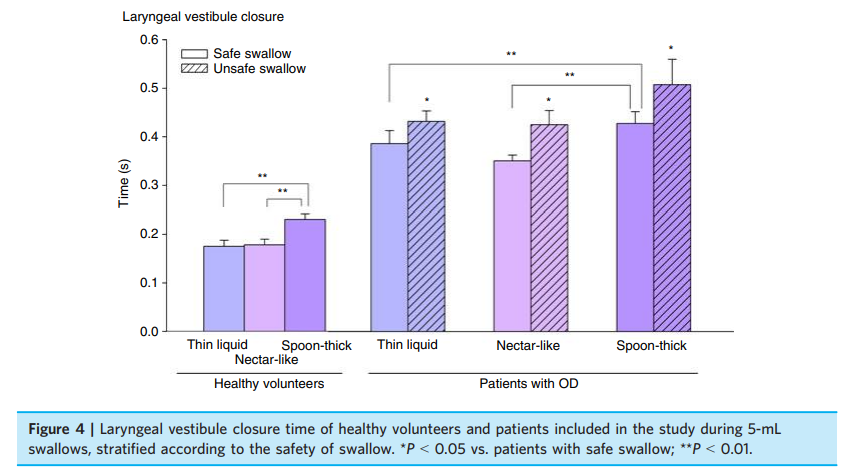
Patients. Timing of swallow response: Overall, patients included in the study presented prolonged swallow response (988.5 21.2 ms, P < 0.001 vs. HV) and delayed airway closure (399.6 19.3 ms, P < 0.001 vs. HV) and UES opening (328.7 14.3 ms, P < 0.001) dur-ing 5-mL liquid swallow. Considering all patients with OD, increasing bolus viscosity to nectar and spoon-thick viscosities did not significantly affect LV closure time (363.1 11.2 ms at nectar viscosity and 434.8 22.9 ms at spoon thick, P > 0.05 vs. thin liquid) or total duration of swallow response (959.3 17.2 ms at nectar viscosity and 1027.1 26.03 ms at spoon thick, P > 0.05 vs. thin liquid). However, time to UES opening was increased at spoon-thick viscosity to 427.5 24.3 ms (P = 0.009 vs. thin liquid). Figure 4 shows time to LV closure of patients stratified according to the safety of their swallow at each viscosity (presence of penetrations or aspirations). Patients with impaired safety presented a delayed LV closure com-pared to patients with safe swallow in all three viscosities (P < 0.05). Patients with safe swallow at thin liquid and nectar-like viscosities had similar timing to airway closure (386.4 26.8 ms at thin liquid and 350.8 11.8 ms at nectar viscosity, P > 0.05), but at spoon-thick viscosity, presented a later time to LV closure (427.8 24.5 ms, P< 0.01) and UES opening.
Bolus kinematics: The mean velocity of a 5-mL thin-liquid bolus (0.248 0.010 m/s) was not changed by increasing bolus viscosity to nectar (0.238 0.010 m/s, P = 0.438), but was significantly slowed at spoon-thick viscosity (0.214 0.010 m/s, P = 0.019 vs. thin liquid).
Figure 2
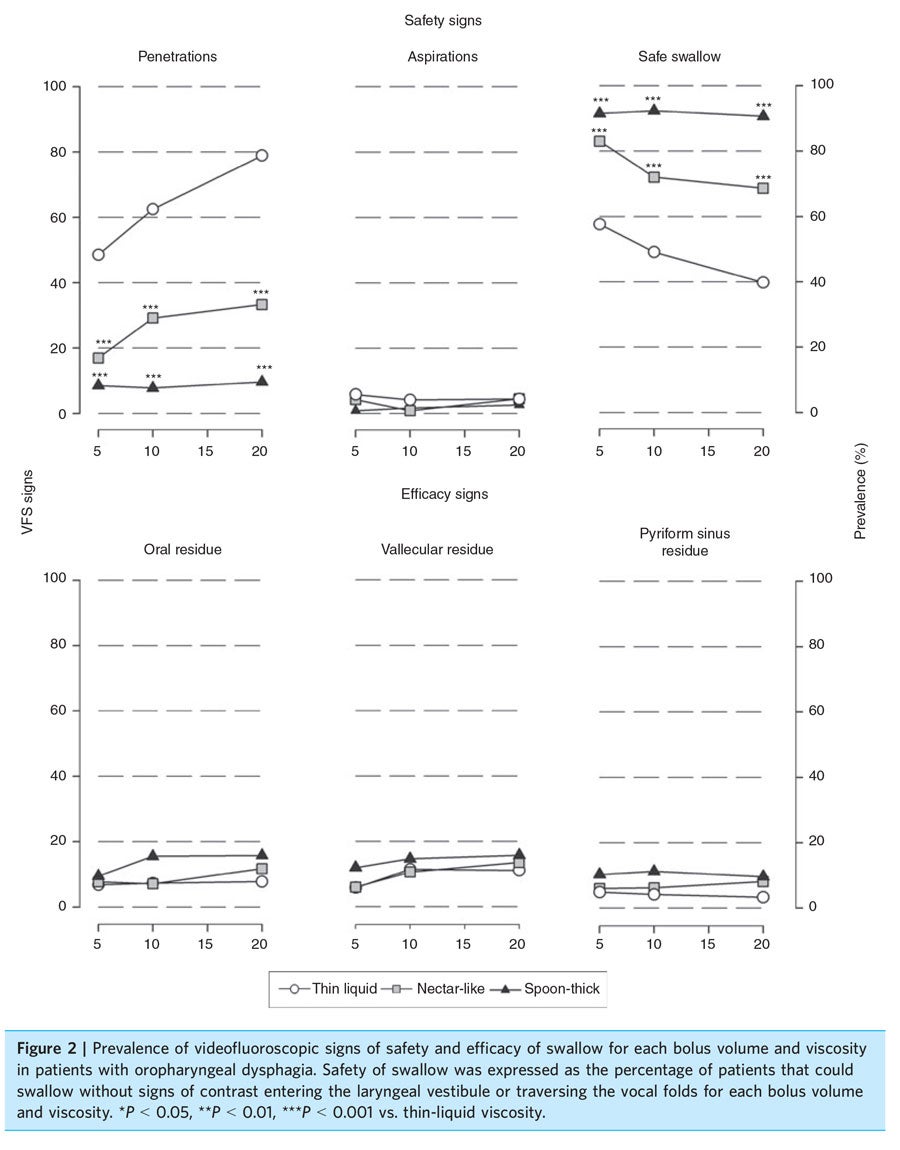
Figure 3
Product safety
A total of 37 minor AEs occurred in 34 (25.4%) subjects during the study and the follow-up period, 30 (25.0%) in patients and four (28.6%) in HV. Of these, 36 AEs were gastrointestinal system disorders, specifically, 33 episodes of loose stools, one of nausea, one of vomiting and one of bloating were registered. The majority of them were mild and not considered treatment related. There was one serious adverse event (bronchoaspiration) that was considered unlikely to be related to the study product but related to the study procedure.
DISCUSSION
The main conclusion of this study is that the new xan-than gum-based thickener, RTUC, presents a strong viscosity-dependent therapeutic effect in patients with OD by improving the safety of swallow without increasing oropharyngeal residue. We found that it is possible to provide safe swallow to more than 84% of patients with OD by using RTUC at spoon-thick viscosity irrespective of the bolus volume offered to the patient. Moreover, prevalence of oropharyngeal residue after deglutition of thickened boluses is significantly lower than those reported in previous studies using starched-based thickeners,2, 9, 18 an advantage of xanthan gum thickeners vs. conventional agents.
Thickening of fluids is a basic strategy in OD management, prescribed to the majority of dysphagic patients.14 Even though a lack of consensus exists in terms of rheological properties, terminology, descriptors and definitions of modified fluids, thickening liquids is perceived as an effective strategy by health professionals providing care for dysphagic patients.14 Despite widespread use and good acceptance, there are few studies objectively assessing the therapeutic effect of thickeners and the level of evidence is low.21 In addition, there are many thickeners and gelling agents commercially available, all presenting different components and rheological proper-ties with potentially different therapeutic effects. Thus, the objective assessment of the real effectiveness of these agents in specific clinical trials is crucial for adequate management of dysphagic patients and to ensure airway protection to avoid respiratory complications. This study shows, for the first time, the strong viscosity-dependent therapeutic effect of a new xanthan gum-based thickener providing research-based evidence of its clinical usefulness in OD management.
In this study, we included patients representing the most prevalent populations and phenotypes of patients at risk for OD that can be found in primary care, general hospitals and nursing homes such as the elderly and patients with stroke and neurodegenerative diseases. Prevalence of malnutrition, comorbidities and polymedication with potential effects on swallowing function among our population was very high, putting them at high risk for developing life-threatening respiratory complications if not managed properly. We previously found that 80% of hospital readmissions for aspiration pneumonia in elderly patients were attributable to oropharyngeal dysphagia.8 One-year mortality rates of our elderly patients with OD are above 50%.2 The RTUC was also evaluated in a group of HV to provide normality values and to obtain data on the effect of the thickener on nor-mal swallow response and its safety profile.
In our study, the therapeutic effect of the thickener RTUC was determined by means of a validated clinical test (V-VST) and a videofluroscopic study. In the clinical study we observed that increasing bolus viscosity reduced prevalence of cough and voice changes associated to swallow, indicating a strong effect on clinical signs of safety of swallow. This effect was confirmed in the video-fluoroscopic study, as a viscosity-dependent reduction in the prevalence of penetrations and aspirations was clearly observed. This therapeutic effect on safety of deglutition exerted by RTUC in this study is higher to that we observed using boluses of similar levels of viscos-ity obtained by starch thickeners in previous studies in patients with neurological diseases (nonprogressive and neurodegenerative),9 a mixed cohort of patients including head and neck diseases18 and in frail elderly patients.2 In terms of efficacy of deglutition, we observed in the clinical study that pharyngeal residue increased at spoon-thick viscosity when compared with thin liquids. However, this effect was not confirmed by the videofluoroscopy. This discrepancy could be explained because in the clinical study, the pharyngeal residue is not a sign directly observed by the clinician but is assessed as a symptom reported by the patient (feeling that the bolus sticks in the throat). Pharyngeal and laryngeal sensory abnormalities, often described in dysphagic patients, could contribute to this symptom. Using videofluoroscopy, we did not observe any significant enhancement in vallecular or pyriform sinus residue by increasing bolus viscosity. These results agree with a previous study in HV that did not find any increase in pharyngeal residue by increasing bolus viscosity with different concentrations of xanthan gum.22 In contrast, previous studies evaluating the effect of starch thickeners,2, 9, 18 reported an important increase in pharyngeal residue at spoon-thick viscosities. Post-deglutitive residue can be easily aspirated in the inhalation process and put the patient at risk for respiratory complications. Therefore, the highest protection offered by the xanthan gum-based thickeners compared with the starch thickeners, together with the absence of pharyngeal residue increment, confers to this new generation of thickeners a greater therapeutic value.
We observed that thin and nectar-like liquids moved more quickly through the pharynx than boluses at spoon-thick viscosity both in HV and in patients. In HV, the timing of reconfiguration of oropharyngeal structures from a respiratory pathway to a digestive pathway adapted to the bolus transit, and the increased bolus velocity of thin and nectar-like liquids was associated with an earlier LV closure and UES opening times. Dysphagic patients presented delayed airway protection (LV closure time), specifically prolonged in patients with impaired safety, responsible for the observed penetrations and aspirations into the airways. It has been pro-posed that slowing down bolus flow velocity through the pharynx confers thickeners their main therapeutic effect.12 However, we have observed that a moderate level of viscosity, such as nectar-like viscosity, strongly improved airway protection without modifying bolus velocity or timing of the oropharyngeal swallow response compared to thin liquids. Therefore, RTUC is able to improve swallow safety without producing any change in swallow physiology, suggesting that the intrinsic proper-ties of the thickened bolus are responsible for the observed therapeutic effect at this level of viscosity. We have also observed that, at spoon-thick viscosity, bolus velocity is reduced, suggesting that at high-viscosity levels, the therapeutic effect of RTUC depends not only on its intrinsic texture properties, but also to additional effects produced by changes in swallow physiology. Looking at the other timing related events, we observed that UES opening time was delayed at spoon-thick viscosity. As the UES requires bolus pressure to open, the reduced velocity of spoon-thick viscosities that thus takes more time to reach the sphincter, delay UES opening time. Total duration of swallow response (time from GPJ opening to LV opening) was not affected by any level of bolus viscosity in HV or in patients.
The therapeutic effect of xanthan gum thickeners vs. starch thickeners at similar levels of viscosity should be further explored by comparative clinical studies, and be based not only on rheological characteristics such as bolus viscosity but also on textural properties such as hardness, cohesiveness, adhesiveness or gumminess, especially at mid-levels of viscosity. It has been reported in post-stroke dysphagic patients that semisolids with high cohesiveness were more likely to accumulate in the pharynx while high gumminess could lead to tracheobronchial aspirations.23 However, data on the effect of these textural properties on the safety and efficacy of swallow are scarce and further studies are necessary to characterise their influence on the effect of thickeners. Finally, results of this study show that RTUC is a safe product with low incidence of AEs. Most of the AEs affected the gastrointestinal tract, were mild and probably related to the X-Ray contrast that causes a well-known osmotic laxative effect on small bowel and enhances colonic motility.
In conclusion, increasing bolus viscosity with the xanthan gum thickener RTUC exerts a strong viscosity-dependent therapeutic effect on patients with OD by improving the safety of swallow without increasing oropharyngeal residue, an advantage of this new generation of xanthan gum thickeners over conventional agents. Our study also suggests that RTUC exerts its therapeutic effect through two sequential mechanisms: at nectar-like viscosity the therapeutic effect relies on the intrinsic rheological or texture properties of the thickener whereas with spoon-thick viscosity, significant changes in swallow physiology also occur.
Figure 4
AUTHORSHIP
Guarantor of the article: Pere Clave.
Author contributions: Rofes, Mukherjee, Swanson and Clave: study concept and design. Arreola: selection of patients. Rofes and Arreola: acquisition of data. Rofes, Arreola and Clave: analysis and interpretation of data.
Rofes and Clave: drafting of the manuscript. Mukherjee: statistical planning and analysis. Rofes, Arreola, Mukherjee, Swanson and Clave: revision for intellectual content. All authors approved the final version of the manuscript.
ACKNOWLEDGEMENT
We would like to thank our patients for their cooperation and all the members of the Dysphagia Team and the X-ray Department of Hospital de Mataro, Nestle Health Science and Nestle Research Center who have participated in this study. We also thank Jane Lewis for English correction.
Declaration of personal interests: PC has served as consultant and received research funding from Nestle Health Science. LR and VA have served as speakers for Nestle Health Science. RM and JS are employers of Nestec Ltd.
Declaration of funding interests: This study was supported by grants from the Spanish Ministerio de Ciencia e Innovacion (PS09/01012, INT 10/228) and Nestle Health Science.
REFERENCES
- World Health Organization. ICD-10 Version:2010 [Homepage on the Internet]. Geneva: World Health Organization, 2010. Available at: http:// apps.who.int/classifications/icd10/ browse/2010/en#/R13. Accessed August 13, 2013.
- Rofes L, Arreola V, Romea M, et al. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil 2010; 22: e230.
- Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke: incidence, diagnosis, and pulmonary compli-cations. Stroke 2005; 36: 2756–63.
- Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003; 60: 620–5.
- Serra-Prat M, Palomera M, Gomez C, et al. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in indepen-dently living older persons: a popu-lation-based prospective study. Age Ageing 2012; 41: 376–81.
- Cabre M, Serra-Prat M, Palomera E, et al. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing 2010; 39: 39–45.
- Almirall J, Rofes L, Serra-Prat M, et al. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J 2013; 41: 923–8.
- Cabre M, Serra-Prat M, Force L, et al. Oropharyngeal dysphagia is a risk factor for readmission for Pneumonia in the Very Elderly Persons: Observational Prospective Study. J Gerontol A Biol Sci Med Sci 2014; 69: 330–7.
- Clave P, de Kraa M, Arreola V, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther 2006; 24: 1385–94.
- Bhattacharyya N, Kotz T, Shapiro J. The effect of bolus consistency on clysphagia in unilateral vocal cord paralysis. Otolaryngol-Head Neck Surg 2003; 129: 632–6.
- Groher ME. Bolus management and aspiration pneumonia in patients with pseudobulbar dysphagia. Dysphagia 1987; 1: 215–6.
- Dantas RO, Kern MK, Massey BT, et al. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol 1990; 258: G675–81.
- Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia 1994; 9: 90–5.
- Garcia JM, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol 2005; 14: 4–13.
- Popa Nita S, Murith M, Chisholm H, Engmann J. Matching the rheological properties of videofluoroscopic contrast agents and thickened liquid prescri-ptions. Dysphagia 2013; 28: 245–52.
- Hjorland B. Evidence-based practice: an analysis based on the philosophy of science. J Am Soc Inform Sci Technol 2011; 62: 1301–10.
- Rofes L, Arreola V, Clave P. The volume-viscosity swallow test for clinical screening of dysphagia and aspiration. Nestle Nutr Inst Workshop Ser 2012; 72: 33–42.
- Clave P, Arreola V, Romea M, et al. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr 2008; 27: 806–15.
- Rosenbek J, Robbins J, Roecker E. A penetration-aspiration scale. Dysphagia 1996; 11: 93–8.
- National Dysphagia Diet Task Force. National Dysphagia Diet: standardi-zation for Optimal Care. Chicago: American Dietetic Association, 2002.
- Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia 2010; 25: 40–65.
- Bogaardt HCA, Burger JJ, Fokkens WJ, Bennink RJ. Viscosity is not a parameter of postdeglutitive pharyngeal residue: quantification and analysis with scintigraphy. Dysphagia 2007; 22: 145–9.
- Momosaki R, Abo M, Kobayashi K. Swallowing analysis for semisolid food texture in poststroke dysphagic patients.J Stroke Cerebrovasc Dis 2013; 22: 267– 70.
L. Rofes*, V. Arreola†, R. Mukherjee‡, J. Swanson§ & P. Clave*,† *Centro de Investigacion Biomedica en Red de enfermedades hepaticas y digestivas (CIBERehd), Instituto de Salud Carlos III, Barcelona, Spain. †Unitat de Proves Funcionals Digestives, Department de Cirurgia, Hospital de Mataro, Universitat Autonoma de Barcelona, Mataro, Spain. ‡Nestle Research Center, Nestec Ltd, L...