ABSTRACT
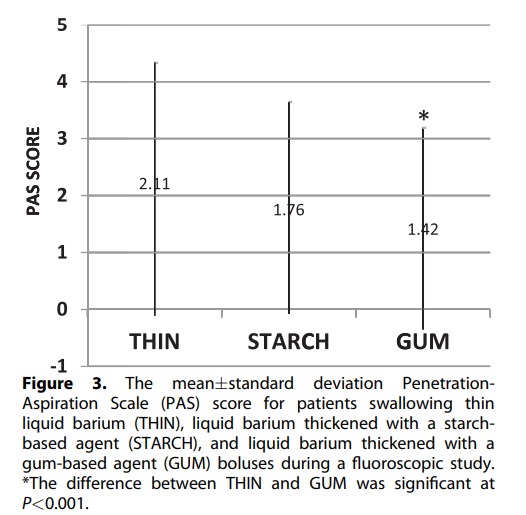
Bolus manipulation is a primary treatment strategy in the management of oral-pharyngeal dysphagia. The use of thickening agents to alter bolus rheology is particu-larly commonplace; however, the precise effects of these alterations on swallowing remain uncertain. The purpose of our study, a prospective, double-blind clinical trial (Level 1b), was to investigate the effects of viscosity on aspiration. One hundred patients with dysphagia were prospectively evaluated with fluoroscopic swallow studies per-formed across three standardized and randomized conditions: thin liquid barium (THIN), liquid barium thickened with a starch-based agent (STARCH), and liquid barium thickened with a gum-based agent (GUM). Outcome measures included the prevalence of aspiration and score on the Penetration-Aspiration Scale. A total of 23 out of 100 patients exhibited 56 episodes of aspiration. Twenty patients aspirated on THIN, 15 on STARCH, and 11 on GUM bolus conditions (P<0.05, thin vs gum). There were 28 in-stances of aspiration on THIN, 16 on STARCH, and 12 on GUM. Mean Penetration-Aspiration Scale score standard deviation was 2.11 2.22 for THIN, 1.76 1.88 for STARCH, and 1.42 1.47 for GUM conditions, respectively (P<0.001, THIN vs GUM). A clinically significant reduction in the incidence of penetration and aspiration was observed for gum-thickened barium compared with thin liquid barium.
J Acad Nutr Diet. 2014;114:590-594.
ORAL-PHARYNGEAL DYSPHAGIA IS ASSOCIATED with many medical conditions, including stroke, neurogenic and neuromuscular disorders, and head and neck cancer. In elderly patients in particular, dysphagia can compromise nutritional status and increase the risk of aspiration pneumonia, leading to significant morbidity and mortality.1,2 Oral nutrition is the desirable goal for every patient with dysphagia, but in some cases may not be possible or appropriate. If adequate nutrition or hydration cannot be achieved, or if aspiration of material into the lungs cannot be prevented, non-oral feeding may be implemented. This alternative is both costly and unsatisfying to many individuals.
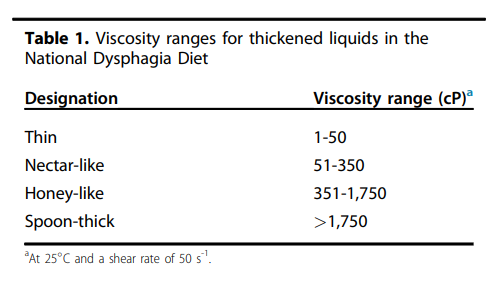
A technique frequently implemented by clinicians attempting to improve swallowing safety in at-risk patients is the manipulation of bolus viscosity. This is particularly considered when patients demonstrate difficulty with thin liquids (eg, water). Foods and beverages may be thickened to consistencies that are judged to be safe and effective based on results of clinical and instrumental assessments. However, few conclusive studies are available to support the wide-spread use of bolus rheology manipulation in clinical practice.3,4 Recognizing the lack of standards related to dysphagia management, in 2002 the American Dietetic As-sociation proposed standardized terminology and definitions of diet modification for patients with dysphagia.5 The Na-tional Dysphagia Diet proposed definitions of solid food textures and viscosity ranges for thin, nectar-like, honey-like, and spoon-thick liquids. The authors suggested liquid viscosity ranges as a framework for future research in this area (Table 1).
Many of the currently available thickening products consist of modified starch. Although starch-based thickeners have been demonstrated to improve swallowing safety and efficiency in patients with dysphagia,6 they have limitations. Starch-based thickeners may not dissolve well in some liquids, can appear cloudy, may taste “starchy,” and may continue to thicken over time.7,8 Viscosity dependence on temperature adds further complexity to achieving a desired level.8
Gum-based thickeners would appear to offer some ad-vantages over starch-based products. Unlike starch, gums (including xanthan gum) are not degraded by amylase in saliva, allowing viscosity to remain stable.9 They are purported to reach target viscosity rapidly, making them well suited to hot beverages, and have been shown to maintain stability in liquids over time.7
Patient acceptability has been shown in an open, observational study of 19 nursing home residents with dysphagia, in which the participants “liked” 94% of drinks modified with a gum-based thickener. The majority of the drinks offered during the study (67%) were fully consumed.10
There have been few systematic efforts to compare the effects of gum-thickened liquids vs thin-liquid or starch-based bolus materials on swallow function.11 The purpose of our investigation was to compare the effects of a thin liquid barium contrast fluid (THIN) to the same barium material thickened with a conventional starch-based (STARCH) and a xanthan gum-based (GUM) thickener in patients with dysphagia. The null hypothesis was that there would be no differences in rates of aspiration across the three bolus types.
Table 1.
METHODS
Subjects
Permission to conduct this investigation was granted by the Institutional Review Board of the University of California, Davis. All adults undergoing a comprehensive dynamic fluo-roscopic swallow study at the Center for Voice and Swal-lowing of the University of California, Davis, between November 2009 and December 2010 were considered for inclusion. Individuals younger than age 18 years and women who were pregnant were excluded from consideration. Written consents were obtained for all patients included in the study. Assuming an aspiration rate of 25% (consistent with data from an Institutional Review Board-approved database of all patients with dysphagia evaluated at the Center since 1998) and a probability of type 1 error of 0.05, it was determined that 100 participants were necessary to provide sufficient power (80%) to detect an improvement in aspiration rate of 10% with the gum- or starch-based agents, compared with thin liquid.
Bolus Preparation
One investigator carefully weighed and prepared all recon-stituted bolus materials immediately before each fluoro-scopic study. Time allowed for thickening was 5 minutes for GUM and 25 minutes for STARCH. For the THIN contrast agent, reconstituted Thin Liquid Varibar 40% wt/vol (E-Z-EM, Inc) was used. This was determined to have a viscosity (at a shear rate of 50 s-1 at 20 C) of 4 to 5 cP. The amount of thickener used was consistent with clinical practice; that is, based on the manufacturer’s recommendations for producing a nectar-thick liquid (4.5 g/100 mL for STARCH; 1.2 g/100 mL for GUM). Calculations were based on the volume of recon-stituted liquid in the standard Thin Liquid Varibar bottles used (ie, 260 mL). Thus, the STARCH contrast agent was prepared by adding 11.8 g Resource ThickenUp powder (Nestlé HealthCare Nutrition, Nestec SA) to the standard bottle of Thin Liquid Varibar 40% wt/vol and subsequently reconstituting the product by adding water. This was deter-mined to have a viscosity (at a shear rate of 50 s-1 at 20 C) of 290 to 330 cP. The GUM contrast agent (Nestlé HealthCare Nutrition, Nestec SA) was prepared by adding 3.1 g of Resource ThickenUp Clear powder to the bottle of Thin Liquid Varibar 40% wt/vol and again reconstituting the product following supplier instructions. This was determined to have a viscosity (at a shear rate of 50 s-1 at 20 C) of 150 to 170 cP. All viscosities were measured using an Anton Paar MCR 500 rheometer (Anton Paar Germany GmbH) using a concentric cylinders geometry over a shear rate range of 0.01 to 100 s-1 except the Varibar Thin Liquid, which was measured between 10 and 100 s-1 due to its low viscosity.
Fluoroscopic Studies
All radiographic studies were conducted at University of California, Davis, by a speech-language pathologist and fluoroscopy technician in accordance with the routine radiographic protocols approved by the institution. Equip-ment used included a properly collimated OEC Medical Sys-tems 9800 Radiographic/Fluoroscopic unit that provided a 63 kV, 1.2 mA-type output for the full field of view mode (12-in input phosphor diameter). Studies were recorded for later detailed review and analysis. Bolus types were pre-sented in random order by the speech-language pathologist conducting the study.
Analyses
Two investigators not involved with the conduct of the fluoroscopic studies and unfamiliar with the order of pre-sentation of the bolus materials independently evaluated the three experimental swallows in all patients. The primary outcome measure was presence or absence of aspiration. A secondary outcome was score on the Penetration-Aspiration Scale (PAS).12 To achieve consensus for analyses, a third investigator evaluated studies where aspiration was disputed, and a majority opinion was used in final tallies. All data were coded and recorded into SPSS 19.0 for Windows (version 2010, IBM-SPSS, Inc). The prevalence of aspiration with GUM and STARCH was compared with the prevalence of aspiration with THIN with the McNemar test. A Friedman test for ordinal data was used to compare PAS scores for the three groups. The Wilcoxon signed-rank test was used to compare each bolus pair. A Bonferroni adjustment was utilized to account for multiple comparisons.
RESULTS AND DISCUSSION
A total of 118 consecutive patients who met the criteria and consented to the study were enrolled. Eighteen participants were discontinued during the fluoroscopic study for their own safety (ie, extreme aspiration risk or inability to manage more than a small bolus). One hundred patients successfully completed the study. Fifty-eight percent of the cohort was men. The mean standard deviation age of the cohort was 62 13 years. A variety of medical conditions contributing to dysphagia was represented in the group. The largest sub-groups included head and neck cancer (23%), history of gastroesophageal reflux disease or foreign body sensation (22%), neuromuscular or neurogenic (20%), medical (eg, connective tissue disease or diabetes) (14%), structural anomaly (eg, osteophyte) (13%), and trauma (8%).
Intraclass correlation coefficients (two-way random effects model) for reliability between the two judges evaluating the studies revealed an agreement of 0.91 for the presence or absence of aspiration and 0.80 for the PAS scores.
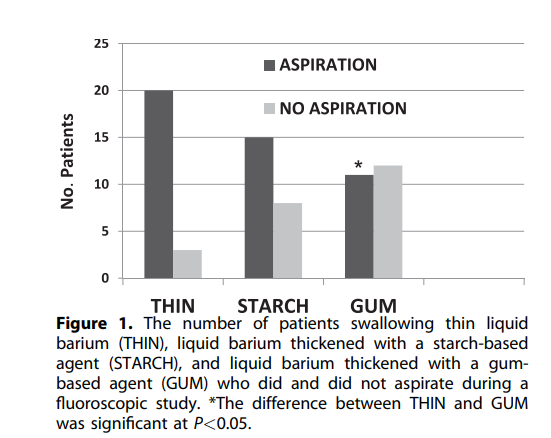
Figure 1.
Aspiration and Bolus Type
Twenty-three of 100 patients demonstrated aspiration on one or more of the three bolus types during the fluoroscopic study. Of 23 patients who aspirated, nine aspirated on three bolus types, five aspirated on two bolus types, and nine aspirated on only one bolus type (Figure 1).
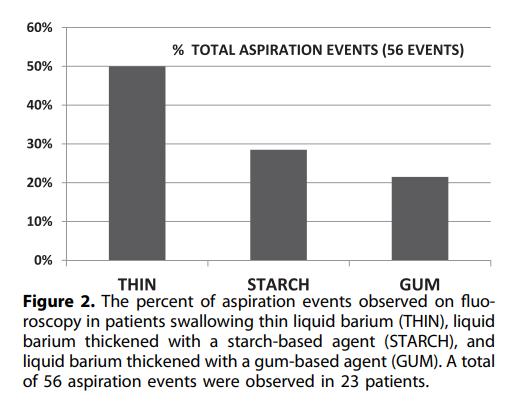
Data presented in Table 2 reveal associations between aspiration and bolus type pairs. A McNemar test revealed a significantly lower aspiration rate for GUM than for THIN (P¼0.016). No significant differences in aspiration rate were found in the comparison between THIN and STARCH (P¼0.18), or between STARCH and GUM (P>0.05). The 23 patients who aspirated demonstrated a total of 56 instances of aspiration. Of these, 28 instances (50%) occurred on THIN, 16 (28.5%) on STARCH, and 12 (21.5%) on GUM (Figure 2).
Table 2.
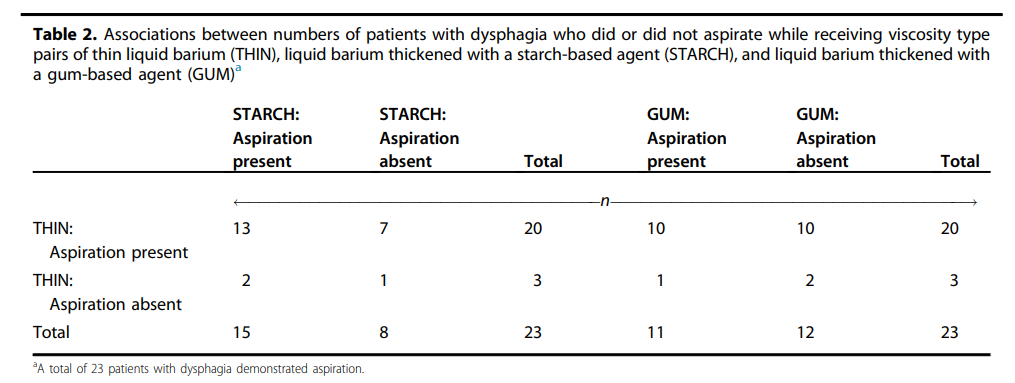
Figure 2.
Penetration-Aspiration Scale
The PAS is an 8-point scale describing entrance of bolus material into the airway, to which level (above or below the vocal folds) and the patient’s response to penetration or aspiration events. A score of one represents no aspiration/ penetration; eight denotes material below the vocal folds with no attempt to eject.12 The numbers of patients in each PAS category, according to bolus type, are presented in Table 3. Means were averaged across judges.
A Friedman test was used to compare the PAS scores by bolus type (three sets of related, ordinal data). There was an overall significant difference in PAS scores according to the three bolus types (P<0.001). The Wilcoxon signed-rank test was used to compare each bolus pair to examine the differ-ences that occurred. A Bonferroni adjustment was utilized to account for multiple comparisons. In this analysis, only GUM vs THIN was statistically significant (P<0.001) (Figure 3).
Figure 3.
Clinicians working with patients with dysphagia frequently manipulate bolus consistency in an attempt to permit safer and/or more effective management of oral intake. Particularly common is the use of thickening agents to prevent aspiration of thin liquids. Although well intentioned, the use of these agents carries certain challenges. Conventional thickening agents are starch-based and, as noted, subject to a number of limitations. The xanthan gum-based thickening agent used in our investigation was developed to overcome limitations in taste, viscosity stability, and solubility associated with starch-based products.
Our study revealed significantly less aspiration on gum-thickened vs thin contrast agent (P<0.05). Although there did appear to be less aspiration with STARCH, compared with THIN, this difference was not significant (P>0.05). In addition to aspiration prevalence, there was also a difference in PAS scores across the three bolus types. PAS scores were significantly lower for GUM than for THIN (P<0.001). The difference between STARCH and THIN was not significant (P>0.05).
Although the reduction in aspiration with GUM vs STARCH did not reach significance, it is important to note the rheologic differences between the starch- and gum-based thickeners, and possible implications for the use of thickeners to support safe swallowing. Commercially available products were used in our study, and the amount of each thickener used was determined by the supplier’s recommendations for producing a nectar-thick liquid. Of particular interest, the thickened sample with the lower viscosity (within the National Dysphagia Diet nectar range), GUM, was associated with less aspiration than the thickened sample with the higher viscosity, STARCH. If increased viscosity were the only variable contributing to improved swallowing safety, this result might be surprising. The clinical differences observed here between the two thickeners are likely related to other rheologic properties of these materials, rather than to viscosity measurements alone. From a rheologic science perspective, thickened foods and beverages are classified as complex fluids, which cannot be adequately described by single values for viscosity and density. For example, the viscosity of a starch- or gum-thickened drink depends on time under flow, and the final steady-state viscosity value depends on the shear rate, or how fast the material flows. An appropriate selection of parameters to describe the properties of a complex fluid during swallowing requires a fluid mechanical analysis of the swallowing process itself. Additional research may clarify the role of these variables in defining the utility of specific bolus materials in patients with dysphagia who are at risk for aspiration. In the interim, it is important for clinicians to recognize the complex relationship between thickening agents and the unique characteristics of swallow function in individual patients and patient populations.
The purpose of our investigation was to compare the effects of THIN fluid to the same barium material thickened with a conventional starch and a xanthan gum-based thickener, respectively, in patients with dysphagia. A similar application of the xanthan-gum thickener to nonbarium materials; that is, to water or juice, may produce comparable advantages in patients, although this remains to be tested. Advantages of xanthan gum related to stability over time and with temperature have, as noted, been previously described. Additional studies are required to further demonstrate patient preference and compliance with the use of GUM. Further research may also elaborate differences in rheologic behaviors within individual National Dysphagia Diet categories; for example, differences across substances that are classified as nectar-thick. A subsequent report will evaluate mechanical differences; that is, timing and displacements observed for swallows of the three bolus types that may further explain findings in our study.
CONCLUSIONS
Our prospective, double-blind clinical trial revealed that in patients we investigated, a gum-based thickener was effective at reducing aspiration, compared with a thin liquid contrast agent. Use of xanthan gum also supports more favorable PAS scores than thin liquid contrast agent. There were no significant differences in aspiration noted between thin barium and contrast thickened to nectar consistency with a starch-based thickener. These findings demonstrate the potential of a gum-based thickening agent to enhance swallowing safety in patients with dysphagia. Further research is needed to evaluate how complex rheologic characteristics of bolus types affect swallowing mechanics, and how these may contribute to swallowing risk and safety in individual patients with dysphagia, and in subgroups of patients; for example, those with cerebrovascular accident or head and neck cancer.
References
- Kaiser M, Bandinelli S, Lunenfeld B. Frailty and the role of nutrition in older people. A review of the current literature. Acta Biomed. 2010;81(suppl 1):37-45.
- Kikawada M, Iwamoto T, Takasaki M. Aspiration and infection in the elderly: Epidemiology, diagnosis and management. Drugs Aging. 2005;22(2):115-130.
- Lazarus CL, Logemann JA, Rademaker AW, et al. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993;74(10):1066-1070.
- Steele C, van Lieshout PHHM. Does barium influence tongue behaviors during swallowing? Am J Speech Lang Pathol. 2005;14(1):27-39.
- National Dysphagia Diet Task Force. National Dysphagia Diet. Stan-dardization for Optimal Care. Chicago, IL: American Dietetic Association; 2002.
- Clavé P, De Kraa M, Arreola V, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24(9):1385-1394.
- Mertz Garcia J, Chambers E, Matta Z, Clark M. Viscosity measure-ments of nectar- and honey-thick liquids: Product, liquid, and time comparisons. Dysphagia. 2005;20(4):325-335.
- Mertz Garcia J, Chambers E, Matta Z, et al. Serving temperature viscosity measurements of nectar- and honey-thick liquids. Dysphagia. 2008;23(1):65-75.
- Hanson B, O’Leary MT, Smith CH. The effect of saliva on the viscosity of thickened drinks. Dysphagia. 2011;27(1):10-19.
- Hibberd J. Acceptance, compliance, and tolerance of a novel xanthan gum-based thickener on oropharyngeal dysphagia patients. Dysphagia. 2011;26(4):432-475.
- Speyer R, Baijens L, Heijnen M, Zwijenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: A systematic review. Dysphagia. 2010;25(1):40-85.
- Rosenbek JC, Robbins J, Roecker EV, et al. A penetration-aspiration scale. Dysphagia. 1996;11(2):93-98.
AUTHOR INFORMATION
R. J. Leonard is a professor, C. White is a senior speech-language pathologist, S. McKenzie is a senior speech-language pathologist, and P. C. Belafsky is a professor, all with the Center for Voice-Speech-Swallowing, Department of Otolaryngology/Head and Neck Surgery, University of California, Davis Medical School/Center, Davis.
Address correspondence to: Rebecca J. Leonard, PhD, Center for Voice, Speech, and Swallowing, Department of Otolaryngology-Head and Neck
Surgery, University of California, Davis, 2521 Stockton Blvd, Suite 7200, Sacramento, CA 95817. E-mail: rjleonard@ucdavis.edu
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
FUNDING/SUPPORT
Financial support for this project was provided by the Nestlé Research Center and Nestlé Health Science (Protocol 09.18.CLI), a wholly owned subsidiary of Nestlé SA, Vevey, Switzerland.
ACKNOWLEDGEMENTS
The authors thank Jan Engmann, Simina Popa Nita (Nestlé Research Center), Maryam Olesen, and Julie Swanson (Nestlé Health Science) for their assistance with this study.
Bolus manipulation is a primary treatment strategy in the management of oral-pharyngeal dysphagia. The use of thickening agents to alter bolus rheology is particu-larly commonplace; however, the precise effects of these alterations on swallowing remain uncertain. The purpose of our study, a prospective, double-blind clinical trial (Level 1b), was to investigate the effects o...