This site is intended only for the use of UK Healthcare Professionals
Season 2
Here you can find all the episodes of our second season with health care professionals. Every week a new episode.
In this podcast Timira Naicker walks us through her journey as a dietitian and how she made the transition into the field of regulatory. Timira gives us great insights about her regulatory dietitian role, what are her interests, what does a typical day looks like and how you can think about a career in regulatory. Disclaimer: BDA endorsement applies only to the educational content of the learning activity.Information for Healthcare Professional Use Only
In this podcast Dr Michelle Harvie discuses the importance of research and setting research questions to test a hypothesis. One particular interesting area of work researched by Michelle is the very low-calorie diet and the 5:2 diet within diabetes. Disclaimer: BDA endorsement applies only to the educational content of the learning activity.Information for Healthcare Professional Use Only
In this podcast Dr Graeme O’Connor discusses his role as a research dietitian and how he made his first research move in the field of refeeding syndrome. After the success of developing clinical guidelines for the management of refeeding syndrome, Graeme went onto to research tube feeding formula containing food derived ingredients at Great Ormond Street Hospital. Graeme also highlights how dietitians can work with industry to test important questions such as 'how can a blended diet work in a hospital setting?' Disclaimer: BDA endorsement applies only to the educational content of the learning activity.Information for Healthcare Professional Use Only
In this podcast Dimitrios Koutoukidis discusses his journey as dietitian from Greece and now in the United Kingdom. His master’s degree enabled him to move into the field of research and is now working on some fantastic research that may support non-alcoholic fatty liver patients in the future. Disclaimer: BDA endorsement applies only to the educational content of the learning activity.Information for Healthcare Professional Use Only
In this podcast Annina Whipp walks us through her experiences as a paediatric and freelance dietitian. What excites her about her role, her interests and the types of projects she gets involved in. Disclaimer: BDA endorsement applies only to the educational content of the learning activity.Information for Healthcare Professional Use Only
Annina Whipp joins us to talk about the ins and outs of setting up a blended diet service. For some, this process isn’t straightforward and there may be several obstacles in the way and things you may not have considered. Annina shares her experiences and reflects on the whole process, sharing her words of wisdom and some helpful tips for others thinking about setting up their own service. Information for Healthcare Professional Use Only
Information for Healthcare Professional Use Only In this episode of the Inside Medical Nutrition podcast, Dr. Linia Patel interviews Ibrahim Amin, a lead practice pharmacist, about his experience managing cow’s milk protein allergy (CMPA). Ibrahim shares his journey into pharmacy, driven by a love for chemistry and a desire for patient contact. The conversation explores the pharmacist's role in cow’s milk protein allergy (CMA) management, emphasising that it extends beyond dispensing prescriptions. Ibrahim discusses supporting patients and healthcare professionals, conducting audits, and ensuring adherence to guidelines. He highlights the importance of recognising that pharmacists are medicine experts and can provide valuable advice. Ibrahim notes a concerning trend of delayed diagnoses and inappropriate management of CMA, often stemming from initial visits to A&E. He stresses the need for accurate diagnoses, appropriate formula prescriptions, and ongoing monitoring of patients. He discusses some of the common symptoms of cow’s milk allergy such as rashes and gastrointestinal symptoms. The discussion delves into the importance of communication and collaboration within a multidisciplinary team. Ibrahim emphasises the value of virtual MDT meetings, which improve efficiency and accessibility. Ibrahim shares practical tips for managing CMA, including reminding parents that "breast is best" and providing guidance on dairy-free diets for mothers who are breastfeeding. The podcast concludes with a call for pharmacists to be proactive in supporting GPs and patients with CMA, emphasising the need for continuous review, accurate diagnoses, and a patient-centred approach. Ibrahim's insights shed light on the crucial role pharmacists play in optimising CMA management and improving patient outcomes. Listen to the full podcast episode to learn more about the role of pharmacists in cow’s milk allergy diagnosis and management. IMPORTANT NOTICE: We believe that breastfeeding is the ideal nutritional start for babies and we fully support the World Health Organisation’s recommendation of exclusive breastfeeding for the first six months of life followed by the introduction of adequate nutritious complementary foods along with continued breastfeeding up to two years of age. We also recognise that breastfeeding may not be an option due to certain medical conditions. Parents should only feed Infant formula for special medical purposes under supervision of a healthcare professional after full consideration of all feeding options, including breastfeeding. Continued use has to be assessed by the healthcare professional in relation to the baby's progress bearing in mind any social and financial implications for the family. Infant formula should always be prepared, used and stored as instructed on the label in order to avoid risks to a baby’s health.
Managing the nutrition and hydration needs of dysphagia patients in the care home setting can be challenging. Sophie Murray Quality Improvement and Regulatory Partner for Signature Care Homes sits down with Linia to discuss optimal management and the positive impact this can have on patient outcomes. Information for Healthcare Professional Use Only
Information for Healthcare Professional Use Only In this episode of the Inside Medical Nutrition podcast, Dr. Linia Patel interviews Claire Thornton-Wood, a paediatric dietitian, about Avoidant Restrictive Food Intake Disorder (ARFID). ARFID is a relatively new diagnosis, recognised in 2013, that encompasses various previous conditions like infantile anorexia and extreme selective eating. It is categorised as an eating disorder, however, unlike other eating disorders, ARFID is not related to body image concerns. Claire emphasises that ARFID is a mental health diagnosis with significant physical implications. It affects both children and adults, with a possible family link. Claire explains that ARFID is characterised by a pattern of avoiding certain foods or food groups, restricting quantities, and not being influenced by body image. The United States Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria include persistent failure to meet nutritional needs, leading to weight loss, nutritional deficiencies, dependence on feeding tubes or supplements, and interference with psychosocial functioning. Predisposing factors include choking episodes, medical conditions causing gagging, tube feeding history, and aversive experiences with medication. The longevity and severity of symptoms of ARFID differentiate this condition from picky eating. Diagnosis of ARFID can be made in both adults and children, with ARFID in children being diagnosed as early as 2 years. The journey to diagnosis can be significant for some children. The impact on families is substantial, causing anxiety about nutrition, social difficulties, and challenges in school. Management involves ensuring nutritional safety, reassurance, and addressing weight concerns. Dietitians may recommend vitamin and mineral supplements, oral nutritional supplements, and fortified foods. In severe cases, tube feeding may be necessary. The end goal is a happy, healthy child and family, with minimal impact on their lives and reduced anxiety. Claire advises healthcare professionals to be alert to ARFID, curious about it, and encouraged by the growing awareness and training in this area. Listeners can find more information on the DSM criteria online, the British Dietetic Association website, and the Nestle N+ Hub. To learn more about the diagnosis and management of ARFID in paediatrics listen to the full episode. Listen to our other episodes of the Inside Medical Nutrition podcast on a range of clinical nutrition topics.
In this podcast Lisa Philips-German, a Paediatric Nurse Consultant talks us through her unique role and how she successfully manages cows’ milk allergy patients in her paediatric community. Lisa will share the success of her clinic and how they have managed to empower and support parents and carers, work with other healthcare professionals and strengthen service provision in the community. Important notice: Mothers should be encouraged to continue breastfeeding even when their infants have cows' milk protein allergy. This usually requires qualified dietary counselling to completely exclude all sources of cows' milk protein from the mothers’ diet. Information for Healthcare Professional Use Only
Dysphagia Chef Gary Brailsford and Independent Dietitian Caroline Hill sit down to discuss texture modified diets. From myth busting to best practice, they explore how to texture modified diets right, for your dysphagia patients. IDDSI Framework * For healthcare professionals only.
To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 0.6 click here. Further reading Management of weight gain in tube-fed children with neurodisabilities Weight Gain in Tube-Fed Neurodisability Children
To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 0.6 click here. Further reading Management of weight gain in tube-fed children with neurodisabilities Weight Gain in Tube-Fed Neurodisability Children
To watch a full webinar on case studies for Peptamen Junior 1.5kcal/ml ONS, from the Acceptability and Tolerance Study, click here. To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 1.5 click here.
To watch a full webinar on case studies for Peptamen Junior 1.5kcal/ml ONS, from the Acceptability and Tolerance Study , click here. To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 1.5 click here.
To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 0.6 click here. Further reading Management of weight gain in tube-fed children with neurodisabilities Weight Gain in Tube-Fed Neurodisability Children
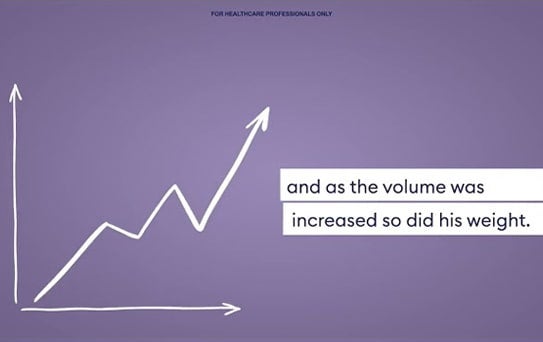
To read and download the case study click here. To read more on the nutritional profile for Peptamen HN click here. Further reading Another case study for Peptamen HN to read and download , click here
To read and download the case study click here. To read more on the nutritional profile for Peptamen HN click here. Further reading C.Dejong; F. Hammargyist et al. ESPEN guidelines on enteral nutrition: gastroenterology. European Journal of Clinical Nutrition Voulme 25, Issue 2. 2006. Pages 260-274. Henry CJK. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutrition 2005; 8 (7A): 1113-1152. Thomas B & Bishop J (Eds.) Manual of Dietetic Practice 4th edition. Blackwell Publishing Ltd; Oxford 2007, pp475-477. K, Spiroglou et al. Gastric emptying in children with cerebral palsy and gastroesophageal reflux. Paediatric Neurology 2004; 31 (3):177-182.
To read and download the case study click here. To read more on the nutritional profile for Peptamen AF click here. Further reading Motor Neurone Disease Association. www.mndassociation.org National Institute for Health and Care Excellence (NICE), (2016). Motor Neurone Disease: Assessment and Management. Available at: https://www.nice.org.uk/guidance/ng42/resources/motor-neurone-disease-assessment-and-management-1837449470149. Ng L, Khan F. Multidisciplinary care for adults with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No.: CD007425. DOI: 10.1002/14651858.CD007425.pub2.
Watch if an enteral tube feed containing food-derived ingredients can improve both the physical health and mental wellbeing of an adult patient. Switching to an enteral tube feed containing food-derived ingredients helped Patient X’s physical health and management, and resulted in great psychological benefits.
To read and download the case study click here. To read more on the nutritional profile for Peptamen Junior 0.6 click here. Further reading Management of weight gain in tube-fed children with neurodisabilities Weight Gain in Tube-Fed Neurodisability Children