GEORGE IS A 63 YEAR OLD MARRIED MAN WHO WAS DIAGNOSED WITH MALIGNANT NEOPLASM OF THE OESOPHAGUS IN SEPTEMBER 2011.
A two stage oesophago-gastrectomy was performed in February 2012 with a jejunal tube inserted for feeding. The patient reported that during his hospital stay he was given a polymeric feed via the jejunostomy. He suffered with severe diarrhoea for the length of his hospital stay. He was discharged home in April 2012, taking small meals and snacks without enteral nutrition.
Over a 6 month period weight loss was recorded as 31% of total body weight. At 6 months a jejunostomy feeding tube was reinstated at home using a peptide feed. Tolerance of the feed was good and the patient’s weight loss slowed and oral diet improved.
Patient’s background, medical history, weight history
George was first reviewed by his local community dietitian in July 2012 after a referral was received by the community dietetic service, requesting an assessment of his nutritional intake and possible enteral feeding.
Along with the diagnosis and treatment of oesophageal neoplasm, a history of chronic obstructive pulmonary disease, asthma, coronary heart disease and type 2 diabetes mellitus were noted at initial consultation. George was also suffering with oral thrush (Candida albicans) of the mouth and oesophagus.
The patient reported his blood glucose levels were currently not being checked at home.
Medications
- Nystatin 1ml qds
- Fluconazole 50mg od
- Lansoprazole 15mg od
- Seretide inhaler
- Ventolin inhaler Metformin 500mg bd
- Ipratropium bromide inhaler
- Amiloride hydrochloride 5mg od
- Furosemide 20mg od
- Aspirin 75mg od
- Simvastatin 40mg od
- Metoclopramide hydrochloride 10mg tds
- Levothyroxine sodium 125ug od
Relevant data/diagnostic tests
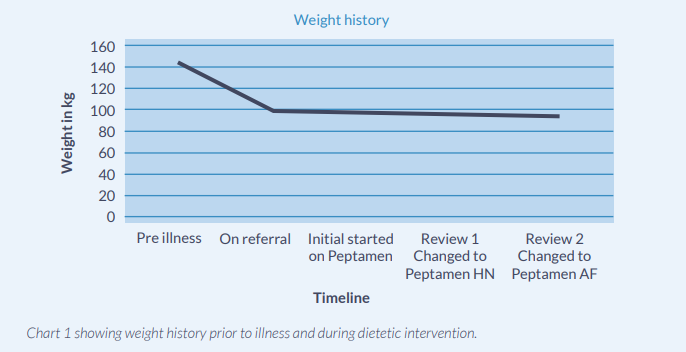
George’s recorded height is 183cm and his weight prior to his surgery was 142.7kg, giving him a body mass index of 42.4 at that time. His weight at referral was 98.8kg (BMI 29.5); this equated to a percentage weight loss of 31% in 6 months. His weight at initial consultation was 95kg (BMI 28.5), he had lost 2kg in 2 weeks (chart 1 below).
Chart 1
Nutritional and Medical Problems
George reported that whilst in hospital he had experienced diarrhoea until the jejunostomy feed was discontinued at his request. Since this time he has been having very small amounts of oral diet. He felt that once home this would improve, however he was still unable to tolerate more than small mouthfuls of food, complaining of symptoms of nausea, vomiting and pain after eating. Consequently his weight decreased dramatically. He tolerates oral fluids well and consumes about 1000ml per day. George is still under the care of the oncology team at the hospital but has been missing appointments; reporting that he felt too weak to leave the house. George had previously tried oral nutritional supplements and didn’t like them. He was unwilling to try them again.
Nutritional problems identified:
- Failure to thrive – loss of weight with significant impact on rehabilitation and activity level
- Food phobia
- Partial loss of appetite
- Post-prandial pain
- Nausea and vomiting
- Reflux
- Dumping syndrome
George complained of feeling weak, being unable to walk more than a couple of steps without tiring, and he felt his quality of life was poor. George was feeling depressed because of his circumstances and was frustrated that he was not recovering faster. George’s nutritional requirements were calculated using a weight of 95kg as follows:1
Energy
13kcal x 95kg + 567kcal
+ 15% added for activity = 2072kcal
Protein
0.17g – 0.2g x 95 x 6.25g = 101g
Fluid
35ml x 95kg = 3325ml
Although his requirements were estimated at 2072kcal and would require 2072ml of a standard 1kcal/ml feed, George was still unsure about the benefits of enteral nutrition and was reluctant to allow it to encroach upon his life. After discussion George agreed to have an overnight feed but only wanted the feed to run for up to 12 hours. The feed would need to run slowly so as not to exacerbate any problems with tolerance. This made it difficult to meet his nutritional requirements.
Nutritional goals/Recommendations
The primary goal of nutritional intervention was to stabilise weight loss and prevent further protein losses.
The secondary goal was also to promote rehabilitation and increase activity.
Initial Feeding Regime
1000ml Peptamen (1kcal/ml) at 83ml per hour for 12 hours overnight 8pm -8am (final rate). This was built up over 4 days from 30ml/hr, to 40ml/hr then 60ml/hr then 83ml/hr. This provided 1000kcal and 40g protein. On the first night George reported that he had his bowels open during the night approximately 4 hours after the feed started. No further problems were reported.
Reviews
After 2 weeks George was reviewed at home. His weight was recorded as 94.8kg (a loss of 0.2kg). There were no problems reported with regards to tolerance with Peptamen. To better meet his requirements of macronutrients, the feed was changed to Peptamen HN (1.3kcal/ml) providing 1300kcal and 66g protein. George was still suffering with oral thrush and his oral intake had decreased to oral fluids only.
After a further 6 weeks George’s weight had decreased to 93.8kg (see chart 1). At this time he had started to eat small snacks throughout the day such as biscuits and pastry. The feed was changed to Peptamen AF (1.5kcal/ml) providing 1200kcal and 76g protein to better meet his requirements for protein. He tolerated this feed well and reported that his bowels were opening once or twice daily. He didn’t report any bloating or discomfort.
Discussion
Following a two stage oesophago-gastrectomy the stomach is smaller and no longer in its original position. Dumping syndrome can occur in some patients due to rapid emptying of ingested food into the duodenum, causing nausea and diarrhoea.2 Conversely, gastric emptying is slowed in some patients because the vagus nerve is transected during the oesophagectomy procedure. In addition, gastric reflux is more likely to occur because of the lack of a gastro-oesophageal sphincter.3 Jejunal oedema due to hypo-albuminaemia can occur.4 There is some thought that this could lead to malabsorption of nutrients. George had a slightly decreased albumin level 3 months after surgery and this was likely to be much more reduced immediately following surgery. This could have been a reason for the diarrhoea that he experienced whilst in hospital. Artificial nutrition support can relieve the pressure on patients to achieve adequate oral intake.
The rationale for choosing Peptamen was twofold. Firstly it was used to prevent any symptoms of intolerance to the feed, there being evidence to suggest that peptide feeds can help reduce the number of episodes of GORD;5 and secondly by doing so to restore George’s faith in enteral feeding.
George had not had a pleasant experience of enteral feeding during his hospital stay and was worried about commencing feeding again. It was important that he viewed feeding in a positive light as it is likely that it will take some time for George to return to a full oral diet. Without an enteral feed to support him through this, he might never reach his full recovery potential.
During the dietetic intervention it was concluded that a change in feed was needed to best meet George’s requirements. Standard Peptamen 1kcal/ml was chosen initially as a starting point to ensure tolerance and to gauge whether oral intake would continue and improve with a supplementary overnight feed. However it became clear that oral intake was not sufficient. George had reservations about changing the feed as he felt he may experience unpleasant symptoms such as diarrhoea. We discussed the options in terms of probable continued weight loss if he remained on Peptamen 1 kcal/ml feed versus his perception of having diarrhoea as a possible symptom if the feed was changed. Studies have shown that changing from 1kcal to 1.5kcal feed helped with weight gain and was tolerated well.6
The decision was left in his hands with the understanding that I would support him regardless of what he chose to do. By this time we had started to build a good working relationship and George understood that I would be available for support and would visit him regularly to review the situation. He chose to have the feed changed and fortunately there were no problems. This helped build his trust so when I suggested the next change of feed there was no resistance.
As illustrated from his weight history (chart 1), weight loss slowed significantly and the primary aim of treatment was met. George is now mobilising more and reports that his mood is much better and consequently has improved his quality of life.
This case report demonstrates the benefits of using a peptide feed for post GI surgical patients on a jejunal feed.
References:
- Henry CJK. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutrition 2005; 8(7A): 1113-1152.
- Law S, Wong J. Cancer of the esophagus. In: Zinner MJ, Ashley SW. (eds.) Maingot’s Abdominal Operations, 11th ed. New York: McGraw-Hill; 2007.
- Kight CE. Nutrition considerations in esophagectomy patients. Nutr Clin Pract. 2008; 23(5): 521-528.
- Farthing MJG, et al. Radiologic features of the jejunum in hypoalbuminemia. AJR 1981; 136: 883-886.
- Khoshoo V, Zembo M, King A, Dhar M, Reifen R, Pencharz P. Incidence of gastroesophageal Reflux with Whey and Caesin Based Formulas in Infants and Children with Severe Neurological Impairment. Journal of Paediatric Gastroenterology and Nutrition 1996; 22: 48-55.
- Khoshoo V and Brown S. Gastric emptying of two whey based formulas of different energy density and its clinical implications in children with volume intolerance. European Journal of Clinical Nutrition 2002; 56: 656-658.
GEORGE IS A 63 YEAR OLD MARRIED MAN WHO WAS DIAGNOSED WITH MALIGNANT NEOPLASM OF THE OESOPHAGUS IN SEPTEMBER 2011.
A two stage oesophago-gastrectomy was performed in February 2012 with a jejunal tube inserted for feeding. The patient reported that during his hospital stay he was given a polymeric feed via the jejunostomy. He suffered with severe diarrhoea for the length of his hospital stay. He was discharged home in April 2012, taking small meals and snacks without enteral nutrition. Over a 6 mo...