
Introduction/overview
A 22 year old gentleman, diagnosed with cerebral palsy (a neurological condition that is specifically caused by problems in the part of the brain responsible for controlling muscles), was referred to the Dietetic department.1
He also had a differential diagnosis of Inflammatory Bowel Disease (IBD), which is the general term used to describe ulcerative colitis and Crohn’s disease. Both these chronic conditions involve inflammation of the gut and it can be very difficult to differentiate between the two conditions. IBD affects as many as 620,000 people in the UK.2
Cerebral palsy can occur if the brain develops abnormally or is damaged before, during or shortly after birth. People with cerebral palsy may also have a number of associated problems including seizures, drooling problems and swallowing difficulties, e.g dysphagia.3
As a result many people with cerebral palsy have communication and learning difficulties, although intelligence is often unaffected. Due to dysphagia this gentleman received all his nutrition and fluid via a gastrostomy tube. He is also registered blind and has epilepsy. The patient was not able to communicate verbally, and as a result his medical decisions were discussed with both him and his mum, who became his welfare guardian.
The patient was seen by the community learning disability team at home and was under the care of the following:
- Psychiatry Department
- Physiotherapy Department
- Speech and Language Therapist
- Dietetic services.
These complex patients require support from multiple professions in order to ensure that all care needs are met.4
Patient’s background and medical history
At school, the patient was originally under the care of a Paediatric Dietitian. When he was transferred to the adult learning disability team in 2011, he experienced the following symptoms:
- long-term diarrhoea
- abdominal pain
- numerous chest infections
- urinary infections
Over the years different feeds were tried: Perative® (Abbott Nutrition) and Osmolite® 1.5 (Abbott Nutrition). Unfortunately neither feed brought about an improvement in symptoms and as a result the patient was referred to the Gastroenterology Department in 2013 for further investigations.
In 2014 the patient received a diagnosis of differential IBD; he underwent investigations to distinguish whether it was Ulcerative Colitis (UC) or Crohn’s Disease (CD). The inflammation was localised in the duodenum, therefore the IBD nurse suspected Crohn’s Disease.
The patient continued to undergo faecal calprotectin tests to determine if it was UC or CD. A colonoscopy showed right-sided changes to the large bowel.
For a CP patient, conducting a colonoscopy is a big procedure because a general anaesthetic is required. Therefore, he was at high risk of developing further complications because of his low body weight and his past medical history.
In 2015 his dietetic care was taken over by myself and at this time the patient was on approximately 800ml of Perative (Abbott Nutrition). Following a hospital admission for a chest infection, his weight continued to decrease. The decision was made to trial a whey-based peptide feed: Peptamen® HN (Nestlé Health Science). Peptamen® HN was chosen due to its unique formulation to help reduce the risk of diarrhoea.5
Due to cerebral palsy, the patient continued to suffer with high tone, which can lead to an increase in metabolic stress. Given the high levels of protein, Peptamen® HN may help to meet requirements. Furthermore it is also made up of 100% whey protein which has been shown to facilitate gastric emptying.6
Peptamen® HN (approx. 1000mls) at 85ml/hour over 12 hours was tolerated and on initiation an improvement was noticed. There was a reduction in the urgency and consistency of the diarrhoea, which was less loose than previously.
In May 2015 it was then decided to increase the feed from 1000ml to 1300ml at 130ml/hr over 10 hours and following this his weight increased.
Soon thereafter the patient developed a chest infection, which caused some weight loss. It was then decided to administer 60ml of Pro-Cal® (Vitaflo) per day, with the aim of increasing this up to 120ml if tolerated. Given that Pro-Cal shot is an energy dense liquid supplement in a low volume, it was deemed as suitable. Unfortunately the diarrhoea increased so his mum requested that the Pro-Cal should be stopped. It was therefore agreed to continue with 1300ml of Peptamen® HN for the next 2 months, until the chest infection cleared and his weight stabilised.
Eventually his weight stablised and mum agreed to the addition of an extra bolus of Peptamen® HN at 1 x 50ml bolus in the morning before pump feeding and an additional 1 x 50ml bolus in the evening; both were well tolerated. It was then agreed to increase the bolus feed further by an additional 2 x 50ml throughout the afternoon, aiming to provide an extra ~600 kcal per day to help promote weight gain.
Nutritional assessment:
BMR – 16.0 x 34kg + 545 = 1,089 kcal x mobility factor 15% (wheelchair bound) plus 10% stress factor, 10% (for active inflammatory bowel disease) = 1,377 kcal for weight maintenance. Additional 600 kcal per day to provide 1,977 kcal for weight gain.
Protein – 0.17 x 34kg x 6.25 = 36g
Fluid – 35 x 34kg = 1,190ml
Nutritional Goals/recommendations
To minimise further weight loss and manage the diarrhoea.
Administration route
- The patient had a MIC-KEY button 16 Fr 1.7cm
- The tube had to be vented before each feed to help release trapped wind
Conclusion
A noticeable improvement in quality of life was observed because the patient was now more involved in his hydro- and rebound therapy.
His mum also observed a big improvement in his mood by noticing more smiles and laughter.
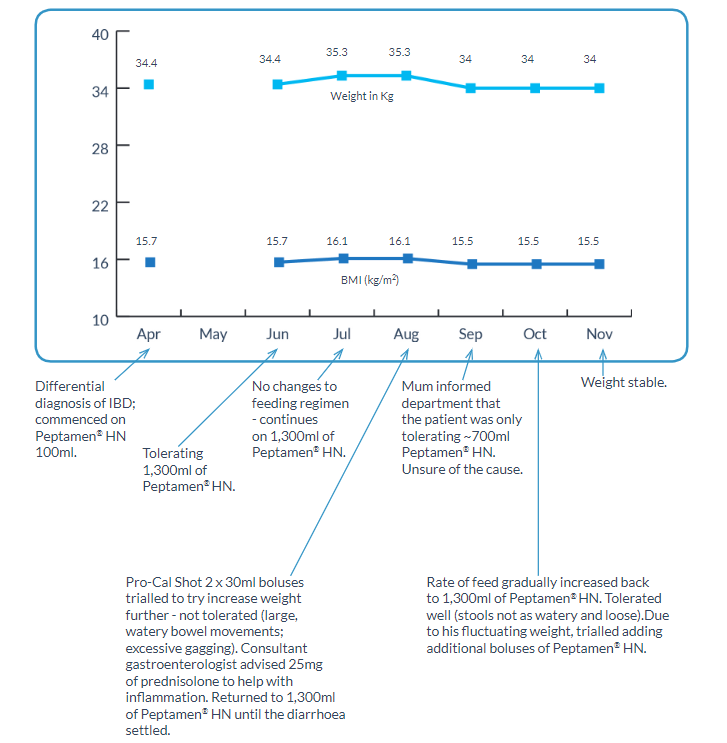
Recently the Consultant Gastroenterologist diagnosed the patient with pancolitis, which is a severe form of colitis and usually means the inflammation has spread throughout the large intestine. Throughout my involvement with this patient, his weight had fluctuated due to various infections and chronic diarrhoea However, for the last 3 months his weight has remained stable.
Peptamen® HN with its unique formulation is also a nutritionally complete feed, with 70% MCT and 100% whey protein, which is suitable for long term use. Given my success with this patient, I can confidently encourage my colleagues to consider using a whey-based peptide feed first line in patients with feeding intolerances.
Summary of weight, nutritional and medical problems
References
1. Cerebral Palsy, NHS Choices (2014). Reviewed at http://www.nhs.uk/conditions/cerebral-palsy/pages/ introduction.aspx. Reviewed on 20th November 2015.
2. Standards for the 2. Healthcare of People who have Inflammatory Bowel Disease (2013 update). Reviewed at http://www.ibdstandards.org.uk/uploaded_files/IBDstandards.pdf. Reviewed on 20th
November 2015.
3. Sleigh G, Brocklehurst P. Gastrostomy feeding in cerebral palsy: a systematic review. Archives of Disease in Childhood 2004; 89(6): 534-539.
4. Borrill.C, West. M, Shapiro. D & Rees. A (2013) Team Working and Effectiveness in Healthcare. British Journal of Healthcare Management, Vol 6, issue 8.
5. Martindale RG, McClave SA, Vanek V W, McCarthy M, Roberts P, Taylor B, Cresci G. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. Society of Critical
Care Medicine and American Society for Parenteral and Enteral Nutrition. Critical Care Medicine 37(5), 1-30 (2009).
6. Khoshoo V, Brown S. Gastric emptying of two whey-based formulas of different energy density and its clinical implication in children with volume tolerance. European Journal of Clinical Nutrition 56, 656-658
(2002).
Background Reading
1. C.Dejong; F. Hammargyist et al. ESPEN guidelines on enteral nutrition: gastroenterology. European Journal of Clinical Nutrition Voulme 25, Issue 2. 2006. Pages 260-274.
2. Henry CJK. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutrition 2005; 8 (7A): 1113-1152.
3. Thomas B & Bishop J (Eds.) Manual of Dietetic Practice 4th edition. Blackwell Publishing Ltd; Oxford 2007, pp475-477.
4. K, Spiroglou et al. Gastric emptying in children with cerebral palsy and gastroesophageal reflux. Paediatric Neurology 2004; 31 (3):177-182.
A 22 year old gentleman, diagnosed with cerebral palsy (a neurological condition that is specifically caused by problems in the part of the brain responsible for controlling muscles), was referred to the Dietetic department.1 He also had a differential diagnosis of Inflammatory Bowel Disease (IBD), which is the general term used to describe ulcerative colitis a...






