
Synopsis
A child (Child M) born premature at 33 weeks and 4 days with a complex secondary diagnosis that included GORD, failure to thrive, IUGR, vitamin D resistant rickets, abnormal vocal cords and chronic lung disease. All of which resulted in the need for increased nutritional requirements. This case study discusses the different feeds that were used to manage the complex feeding intolerances and eventually Child M’s improvement on Peptamen® Junior.
Introduction/Overview
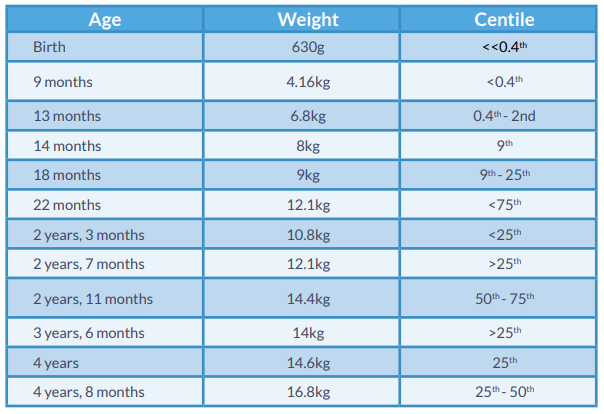
This case study outlines the feeding challenges experienced by an ex-premature, 4-year old girl. She had a number of diagnoses including: twin-to-twin transfusion, intrauterine growth restriction (IUGR), gastro-oesophageal reflux (GOR), metabolic bone disease (MBD) and failure to thrive (FTT).
Prematurity has a prevalence of 50% in twin-pregnancies, and may have an impact on an infant’s development both in utero and after birth.1 This can lead to delayed development and growth, resulting in difficulties with feeding ability and tolerance. GOR is one of the many conditions that is specifically linked to prematurity and the National Institute for Health and Clinical Excellence (NICE) recommend enteral feeding if a child has faltering growth, regurgitation and other channels of management, both medical and dietary, are unsuccessful.2
This case study highlights the difficulties of establishing feeding tolerance to various enteral feeds and the route taken to promote healthy weight gain while addressing feeding intolerance, as monitored by a specialist enteral nutrition team.
Patient’s Medical History & Diagnosis
- Current diagnoses of Child M are:
- Prematurity (33 weeks, +4 days)
- GOR
- Twin-to-twin transfusion
- Metabolic bone disease
- FTT
- IUGR
- Vitamin D resistant rickets
- Chronic lung disease (CLD)
- Hyperbilirubinemia
- Brachy-plagiocephaly
- Delayed development
Prior to community referral, she was seen by a tertiary hospital’s neonatal dietetic team, in conjunction with multiple specialist medical teams. Weight gain was complicated by difficulty in tolerating feeds as well as having an unsafe swallow, thus oral intake was limited.
Once home, her stools were watery and very frequent. Prior to discharge Child M had multiple investigations, including nutritional blood screening and endoscopies, with no reported abnormalities. After discharge stool samples were taken and showed no infections present. A review by the respiratory team resulted in a diagnosis of abnormal vocal cords. Child M remains under the care of the gastroenterology and respiratory medical teams due to the ongoing problems.
Child M was then referred to the local enteral nutrition team with a gastrostomy in place at 9 months of age. It has since been changed to a button gastrostomy. She had moderate tolerance of a high calorie infant contract formula, but regularly had loose stools (more than 10 times per day) which only worsened days after discharge. This then continued over a period of one year. Around her first birthday she developed gas and bloating with abdominal distention. Soon after this she began to struggle with vomiting and her reflux became more prevalent.
Medications
- Omeprazole
- Azithromycin
- Glycopyrrolate
- Movicol® (Laxative)
- Sytron® (Iron Supplement)
- Dalivit® (Multi-vitamin)
Nutritional Intervention
Aims/Objectives:
- Ensure catch-up growth and subsequent healthy weight-gain achieved (tracking on 25th centile, in line with length)
- Feeding tolerance and moving towards safe oral intake
To meet nutritional requirements 120-130 kcal/kg/day and 120ml/kg/day to achieve catch-up growth and maintain hydration status, as per current recommendations3
Child M was initially on a high calorie infant formula. Post discharge her tolerance reduced, resulting in >10 loose, watery stools each day. Initially feed rate was reduced, aiming to improve tolerance.
The following feeding regimen were trialled:
- Feeding regimen 1
- High calorie infant formula 4 x 55ml, gravity bolus feeds and 300ml @30ml/hour
- Feeding regimen 2
- High calorie infant formula 4 x 55ml @55ml/hour and 300ml @30ml/hour via pump. This resulted in little change, following advice based on the aim of decreasing frequency of feeds to minimise gastric stimulation.
- Feeding regimen 3.
- High calorie infant formula 3 x 75ml @75ml/hour and 1 x 300ml @30ml/hour. This led to improved bowels, reducing her stools to 4 times a day. Concurrently Child M started to show signs of possible reflux with coughing during feeds and small possets of milk at times.
Over the following 2 weeks, her loose stools started again with around 8 per day. She was then placed on a peptide-based, energy dense (1.5 kcal/ml) feed. After 2 weeks on the new feed, mum discontinued the feed as no difference was observed. She was then placed back on her previous feed, but struggled with the higher volume which was needed to ensure a healthy weight gain.
Timeline: Age 1 - 5 years
Age 1
At one year of age Child M was gaining weight well and approaching the 0.4th centile. She continued on the high calorie feed with fluctuating bowel movements ranging from 4-8 wet stools per day. Over time, she struggled with increasing gas and bloating. This pattern continued for the next few months, but her weight gain was consistent.
Age 1 ½
At 18 months old, a 1 kcal/ml standard feed (for over 1 year olds) was trialled. This was tolerated, in a similar manner to previous feeds, with no increase, but also no decrease, in her bowel movements and vomiting episodes.
Age 2
At 2 years of age her feed was switched to a 1 kcal/ml semi elemental, nutritionally complete tube feed. Initially it appeared to resolve her loose bowels which decreased from 7 x watery stools to 4 x watery stools per day.
A NISSEN procedure was carried out and the reflux was resolved at this time. After a month on this feed, Child M experienced extreme loose stools and was thus given half Dioralyte® and half of the feed volume to prevent dehydration.
Stool samples were taken and investigations were carried out, which showed no abnormal results. Her feeding regimen was changed to a slower rate overnight, however the same symptoms reoccurred and her parents switched her back to the 1 kcal/ml standard feed. Some improvements were reported temporarily. The following feeds were also tried from time to time and the parents were making the changes without any dietetic input:
1.5 kcal/ml tube feed or 1.5 kcal/ml tube feed and 1 kcal/ml tube feed
1.5 kcal/ml tube feed enriched with 0.8g/ml fibre (50% soluble, 50% insoluble)
This would happen over a period of a few months and was regularly changed by the parents.
Age 3 ½
At the age of 3½ years, Child M then experienced her first vomit since the NISSEN procedure. At this point she had an impedance study and reflux was confirmed. The gastroenterology team discussed a jejunostomy tube due to the ongoing significant reflux of unknown cause. These symptoms were very distressing and caused great concern for her mum.
After 2 months Child M experienced ongoing watery/loose stools and reflux, it was then decided to trial 2 x 150ml of Peptamen® Junior Liquid (PJL) and 2 x 100ml of Peptamen® Junior Advance (PJA). These feeds are known to be isotonic, in other words closer in osmolality to the bodily fluids. In addition, whey based feeds may help with gastric emptying.4
Age 3 ½ - 4
Within a month her feeding tolerance was much better and there was a marked improvement in her stool consistency, moving towards formed stools. This then started to present as constipation. It was queried whether toilet training was an underlying issue after the long-standing difficulties with loose stools and minimal bowel control development. The dietetic department educated parents around toilet training and advised on increasing her fluid intake. Child M was then started on a laxative every second day and opened her bowels every third day. There was no straining and overall she was clinically improved, with no vomiting or excess fluid losses and she was opening her bowels on her own. She continues on a laxative in varying volumes, depending on her stool pattern.
Due to the larger volumes of feed given for weight gain, Child M experienced an episode of vomiting. It was then decided to change the feed to 4 x 100ml of Peptamen® Junior Advance to avoid any unnecessary increases in volume of feed, however she was still receiving water flushes for medication.
Age 5
Child M is now 5 years of age, with a gastrostomy tube in situ, and tolerating 4 feeds a day. The mum was happy and reported that she saw the first normal “poo” after many years of struggling. Her quality of life has improved and she is able to partake in more school activities. In addition, quality of life has also improved for the family, given that mum now has more time on her hands to focus on herself and her daughter’s twin sister.
Conclusion
In 4 years of medical and nutritional interventions, and years of struggling to diagnose Child M’s reason for chronic feeding intolerance, no long-term solutions were found. After trialling Peptamen® Junior and Peptamen® Junior Advance, the balance of high energy, easy absorption and isotonic formula appeared to be the solution to minimise Child M’s feeding difficulties. Months after starting these feeds she rarely struggles with loose stools and continues to thrive.
References
1. National Institute for Health and Clinical Excellence (NICE) Multiple pregnancies: Twin- and Triplet-Pregnancies, NICE September 2013.
2. National Institute for Health and Clinical Excellence (NICE) Gastro-oesophageal reflux disease in children and young people: diagnosis and management, NICE January 2015.
3. Clinical Paediatric Dietetics, 4th edition. Ed Shaw V, 2014. Wiley, Blackwell, Oxford.
4. Khoshoo et al. (1992).Decrease in gastric emptying time and episodes of regurgitation in children with spastic quadriplegia fed a whey-based formula. J Pediatr 1992;120:569-72.
A child (Child M) born premature at 33 weeks and 4 days with a complex secondary diagnosis that included GORD, failure to thrive, IUGR, vitamin D resistant rickets, abnormal vocal cords and chronic lung disease. All of which resulted in the need for increased nutritional requirements. This case study discusses the different feeds that were used to manage the complex feeding ...













